Fundal Height: Why Is My Doctor Measuring My Belly?
During pregnancy, your provider will monitor your overall health and keep tabs on your growing bump. One way they’ll assess baby’s development and growth in-utero is by measuring fundal height. But exactly what is fundal height, and what can it reveal? Keep reading to learn from ob-gyns and midwives everything to know about normal fundal height by week, if and how to measure it at home and more.
Fundal height is a measurement taken in pregnancy that’s used to track baby’s size, growth and positioning in a non-invasive way. Essentially, providers look at the size of your uterine fundus (the uppermost and widest part of the uterus where baby grows) to gauge baby’s size and development. “It’s a screening tool to identify babies that may have growth concerns,” explains Stephanie Hack, MD, ob-gyn and host of the Lady Parts Doctor podcast. “It can indicate if the pregnancy is progressing normally and can help identify potential issues like growth restrictions (a smaller-than-normal baby) or macrosomia (a larger-than-normal baby).”
Fundal height can also be used to help providers track your amniotic fluid levels, adds Rebekah Mustaleski, CPM-TN, a certified professional midwife and compression director with Motif Medical.
When do providers start measuring fundal height? They usually start taking measurement of fundal height between 20 and 24 weeks, as this is when the uterine fundus measurement begins to “correspond well to the gestational age of the pregnancy in weeks,” explains Christina Pinnock, MD, an ob-gyn at Stanford Medicine Children’s Health. This is also when the top of the uterus typically begins to align with Mom’s belly button.
The fundal height measurement is usually taken in centimeters with a tape measure during prenatal checkups later in the second trimester and throughout the third, Hack says. Your provider will measure from the top of your pubic bone to the highest point of your uterus.
Since fundal height is measured with a tape measure, you may be wondering how to measure fundal height at home—and if it’s okay to do so. While you can certainly take measurements for “personal interest,” it’s important to have it professionally measured during prenatal visits for accuracy’s sake, Hack says.
If you do want to try it for your own curiosity, experts recommend using a soft tape measure almond following these steps:
- Place the zero on top of your pubic bone
- Stretch the tape up and over your uterus
- Try to keep the tape measure straight and parallel to the floor
- Check the measurement
“Be aware that being able to feel the top of the uterus and accurately measuring is a simple process, but it’s also a skill that might take time for you to learn,” says Mustaleski.
Because measurement of fundal height is used to approximate fetal size, any conditions that impact uterine size can also impact fundal height, Pinnock says. According to the Cleveland Clinic, this includes conditions like:
- Too much or too little amniotic fluid
- Uterine fibroids or cysts
- Anatomical anomalies, like a reverted uterus
- A larger or obese body mass index
- A pregnancy of twins or multiples
- Baby’s growth rate in-utero
- Baby’s positioning
According to Hack, while measuring fundal height is a useful screening tool, it’s not definitive. “Its accuracy can vary and is less reliable for predicting specific issues compared to ultrasounds. However, it’s valuable for tracking general growth patterns over time,” she says. Pinnock agrees, adding that fundal height measurements have an error range of up to plus or minus 3 centimeters.
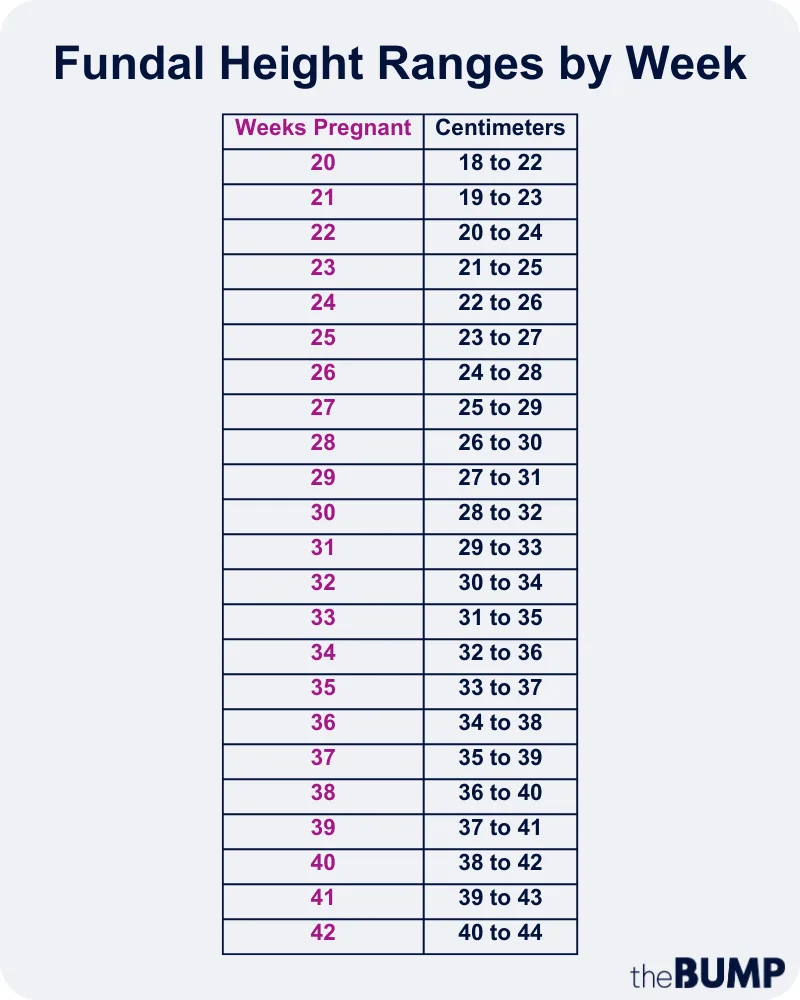
Experts note that a range of plus or minus 2 centimeters in baby’s fundal height compared to weeks of gestation is typically normal. “Typically, the fundal height in centimeters roughly corresponds to the week of pregnancy from weeks 20 to 37,” Hack explains. “For example, at 24 weeks, the fundal height is usually around 24 centimeters, but 22 to 26 could be acceptable.”
Fundal height chart
Wondering what ranges are normal for fundal height by week of pregnancy? Check out the handy fundal height chart below:
If baby’s fundal measurements continue to be 4 centimeters too big or small compared to their gestational age in weeks, it may point to a specific condition, like intrauterine growth restriction (fundal height measuring small) or gestational diabetes (fundal height measuring large), Pinnock says. If baby’s fundal height measures big or small, the next step is to get an ultrasound to get a more accurate grasp on baby’s weight and size and your amniotic fluid levels.
“Fundal height decreases rapidly in the first few days postpartum and isn’t typically measured, as the focus shifts to postpartum recovery,” Hack says. But if you’re curious, the process of the uterus shrinking back down to its non-pregnant size after childbirth is called involution. According to Mustaleski this process starts within minutes of baby being born, and continues over the course of a few weeks. “During the first few days after delivery, the uterus will continue to shrink at a rate of around one centimeter per day,” Pinnock adds.
Shortly after birth, the uterus moves to a position right above or below the belly button. By the end of the first week postpartum, it shifts somewhere between the belly button and the pelvic bone. By the second week postpartum, the uterus is typically found in the pelvis, and you’re no longer able to feel it, Mustaleski says. By the end of six weeks postpartum, your uterus should fully shrink back to its non-pregnant size, Pinnock adds, which is around 60 grams compared to “1000 grams immediately postpartum.” She does caveat, though, that having a larger uterus prior to childbirth, based on factors like extra amniotic fluids or a multiples pregnancy, may affect how quickly the uterus shrinks back.
Fundal height is just one way your provider evaluates the well-being of your pregnancy and baby. “It’s important for expectant mothers to attend all prenatal appointments and always discuss any concerns or anomalies with your healthcare provider to ensure the best care for you and your baby,” says Hack.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Stephanie Hack, MD, MPH, is board certified ob-gyn and host of the Lady Parts Doctor podcast. She obtained her medical degree from Lewis Katz School of Medicine at Temple University, as well as a masters degree in public health. She completed her residency at Georgetown University Hospital and Washington Hospital Center.
Rebekah Mustaleski, CPM-TN, IBCLC, is a certified professional midwife specializing in evidence-based maternity care. She co-founded Roots & Wings Midwifery in Knoxville, Tennessee. Mustaleski received her bachelor’s degree in psychology from Centre College and worked as a doula and birth photographer prior to establishing Roots & Wings.
Christina Pinnock, MD, is an ob-gyn at Stanford Medicine Children’s Health and clinical instructor in maternal fetal medicine at Stanford Medicine. She earned her medical degree from SUNY Downstate College of Medicine and completed her residency at Stony Brook University.
Cleveland Clinic, Uterus, March 2022
Learn how we ensure the accuracy of our content through our editorial and medical review process.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.