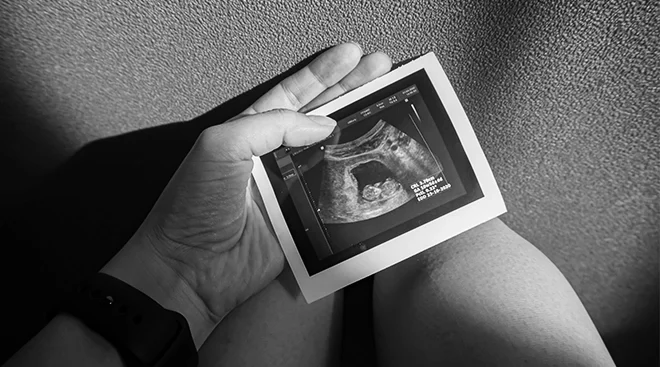
13 Different Types of Miscarriage and What They Mean
It’s an alarming statistic, but one that’s important to know: According to the American College of Obstetricians and Gynecologists (ACOG), up to 26 percent of all pregnancies end in miscarriage—and many women don’t even know they’ve had one. Medically known as a “spontaneous abortion,” miscarriage is defined as the loss of pregnancy before 20 weeks of gestation.
Some miscarriages are unmistakable, marked by bleeding and intense cramping. But sometimes, early pregnancy loss is a much quieter experience; it may even go undetected. “Probably half of my patients present with bleeding and cramps, and the other half have no real symptoms—they come in for a routine prenatal visit and then we find it,” said Melissa Helmich, MD, an ob-gyn and assistant professor for the department of obstetrics and gynecology at the University of Arkansas for Medical Sciences. Moreover, a miscarriage can happen before you even know you’re pregnant, so you might mistake bleeding as your regular period.
The big takeaway doctors want you to know: A miscarriage isn’t your fault. There’s really nothing you can do to avoid a pregnancy loss, says Sheila Mody, MD, an ob-gyn affiliated with UC San Diego Health. Most occur because the fetus isn’t developing as expected, due to chromosomal abnormalities that happen by chance. Still, knowing what’s happening to your body and understanding the different types of miscarriage can go a long way in helping you heal emotionally. Below, the most common types of miscarriage—and what they mean.
If you’re pregnant and experiencing bleeding or cramping but an ultrasound shows that your cervix is closed and baby still has a heartbeat and is considered viable, there may be the threat of possible miscarriage. Of course, this can be incredibly scary to learn. Research shows that about 50 percent of these cases result in miscarriage. The good news: That means the other 50 percent “go on to have a healthy and happy pregnancy,” says Helmich.
Helmich explains that a miscarriage is considered unavoidable—thus, inevitable—if bleeding and cramping increase, and a pelvic exam shows that the cervix is open. Your doctor will discuss the options for care to get you through this unfortunate event. This may include going home to wait it out, taking medication or having a surgical procedure, called a dilation and curettage (D&C), to remove tissue from the inside the uterus and move the process along in a safe way.
A clinical miscarriage is a generic term used to describe a case where pregnancy was clinically proven to exist, either via a positive pregnancy test or an ultrasound, but is no longer viable. This encompasses many other types of miscarriage.
If you get a positive pregnancy test result at home and then subsequent tests turn up negative—or you start bleeding around the time your period was due—you may have experienced a chemical pregnancy. This is a pregnancy that doesn’t progress and is lost shortly after implantation. According to the Cleveland Clinic, chemical pregnancies tend to happen within the first five weeks of pregnancy—so early that many people who miscarry this way never even realized they were pregnant in the first place. The American Pregnancy Association estimates that chemical pregnancies account for 50 to 75 percent of all miscarriages.
A missed miscarriage is exactly what it sounds like. There’s no telltale bleeding or pain. It’s usually diagnosed during a routine prenatal appointment or ultrasound. “People can come in with no signs or symptoms, expecting everything to be healthy, and then we don’t hear or see a heartbeat,” says Jessica Anderson, CNM, director of midwifery services at the University of Colorado College of Nursing. “That’s always a hard situation.”
A miscarriage is considered complete when there’s bleeding and cramping and, on its own, the body “expels the entire pregnancy content,” explains Anderson. This may happen at home—and there may be some blood clots. In this instance, you most likely wouldn’t need any other treatment.
When someone is actively miscarrying—they’re pregnant and experiencing symptoms of bleeding and cramping—and their doctor can tell that the pregnancy is no longer viable, the body may need help passing every bit of fetal or placental tissue out of the uterus. In this instance, a doctor may prescribe medicine or recommend a D&C to ensure that everything comes out, says Anderson.
Recurrent pregnancy loss is when a person experiences more than one miscarriage, says Mody. Typically, a doctor won’t order a full workup until after a second miscarriage. “When you consider that one in four pregnancies might end in pregnancy loss, two miscarriages can be very normal,” adds Helmich. Bloodwork—which includes zeroing in on your antibody levels—will show if there’s something medically going on that needs to be addressed to ensure healthy future pregnancies, notes Anderson. Doctors may also prescribe a hysterosalpingography—essentially an X-ray of the uterus that can detect if it’s abnormally shaped.
A blighted ovum, also known as an anembryonic pregnancy, means there’s an empty sac with no heartbeat and no fetal pole, explains Anderson. It occurs when a fertilized egg implants and an embryonic sac forms and grows, but the embryo fails to develop.
A septic miscarriage occurs when a pregnant person contracts an infection inside their uterus shortly before or after the body starts to miscarry. It’s incredibly rare, says Mody. Fever, chills, pelvic pain or white discharge can be signs of an infection, which needs to be treated right away. If you’re going through a miscarriage at home, be sure to report any symptoms to your doctor.
If a doctor previously confirmed twins or multiples but can’t detect a second (or third) embryo during a subsequent ultrasound, it’s likely due to vanishing twin syndrome. This is where pregnancy doesn’t progress for one of the embryos, says Anderson. It likely stopped developing and became absorbed into the mom or surviving embryo.
As explained by Mayo Clinic, a molar pregnancy is a rare complication characterized by the abnormal growth of trophoblasts, cells that typically form the placenta. Molar pregnancies usually result in a miscarriage; sometimes a D&C is required.
The ACOG considers pregnancy loss before 13 weeks an early miscarriage. Most of the types of miscarriage mentioned above happen early. A late miscarriage is one that occurs after 13 weeks but before 20 weeks, at which point it’s considered a stillbirth. Most of the above types of miscarriage would be considered early. This all may sound alarming, but the reassuring news is that the risk of miscarriage decreases after baby’s heart has been detected around the 8-week mark and continues to fall as the weeks progress.
Knowing the types of miscarriage can help educate and empower you in the unfortunate event of pregnancy loss. But that’s just the start of your journey. Once it’s been established that you’re having or have had a miscarriage, “we make a lot of shared decisions,” says Mody. If your pregnancy doesn’t pass on its own, you and your doctor will determine the best path forward: letting your body handle it at home, taking medication to induce the passing of all fetal material or having a D&C.
It usually doesn’t take long for your body to be physically ready for what’s next, whether that’s trying for another pregnancy or going right onto birth control, says Helmich. Mental healing may take longer, though. Experts generally agree that turning to your support system is important. “What we hear from patients is that talking to someone who has experienced pregnancy loss—someone who has been in their shoes—is really helpful,” says Mody.
What’s more, being open about miscarriage helps to normalize pregnancy loss. “The moment that pregnancy test turns positive, you’re thinking about how this baby will fit into your life,” says Helmich. “When you lose that pregnancy and all those plans you’ve made suddenly have to change, normalizing your grief and the feelings you’re having is important.”
About the experts:
Jessica Anderson, CNM, is the director of midwifery services at the University of Colorado College of Nursing. She received her doctorate in nursing from there as well.
Melissa Helmich, MD, is an ob-gyn and assistant professor for the department of obstetrics and gynecology at the University of Arkansas for Medical Sciences. She received her medical degree from the University of Arkansas for Medical Sciences.
Sheila Mody, MD, is a family planning specialist and an ob-gyn affiliated with UC San Diego Health. She earned her medical degree from the University of Michigan Medical School.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.