How to Spot (and Even Prevent) Food Allergies in Babies
Giving baby their first tastes of solid foods is pretty exciting (and messy). But it can also bring on a fair amount of anxiety for parents—not only do you have to be on the lookout for signs baby is choking, but you also want to keep an eye out for any indications that baby is having an allergic reaction to something they’ve eaten.
It used to be recommended that parents keep potential allergens out of baby’s diet until they were one year old, but thanks to evolving knowledge, we now know that the best way to prevent baby from developing a food allergy is to give them potential allergens early and often. So what are the common food allergies in babies, what causes them and what are the signs of a food allergy in baby to be on the lookout for? We tapped Jonathan Spergel, MD, a pediatric allergist and immunologist and the chief of allergy section at Children’s Hospital of Philadelphia, to give you all the answers.
Food allergies in babies are a serious condition—just one accidental exposure can potentially have life-threatening impacts. A food allergy is an immune system response to an allergenic food. When a food allergic reaction occurs, your child’s immune system is treating a potentially allergenic food as a foreign invader, and the reaction is a result of their immune system overreacting to an otherwise harmless food. One in 13 children suffer from a food allergy in the US—that’s almost two in every classroom.
IgE-mediated vs. non-IgE mediated allergy
IgE-mediated food allergies are the most common type of food allergies in babies, and cause your child’s immune system to react when exposed to an allergenic food. Immunoglobulin E (IgE) antibodies are the cause of this reaction, which usually occurs immediately after your little one ingests the allergen. Symptoms of IgE-mediated reaction include hives, coughing, wheezing or vomiting and occur within minutes to two hours after exposure (for more details, see below).
However, there is another type of food allergy that is less common but can also be found in children: a non-IgE-mediated allergy. With a non-IgE-mediated allergy, the reaction is caused by other parts of the immune system. The reaction—which typically involves the gastrointestinal tract—is often delayed and can take up to two days to develop.
Food allergy vs. food intolerance
While food allergies involve your immune system, food intolerances are adverse health effects caused by foods that do not involve the immune system. The term “food intolerance” is often used interchangeably with the term “food sensitivity.” Unlike a food allergy, a food intolerance is rarely ever life-threatening.
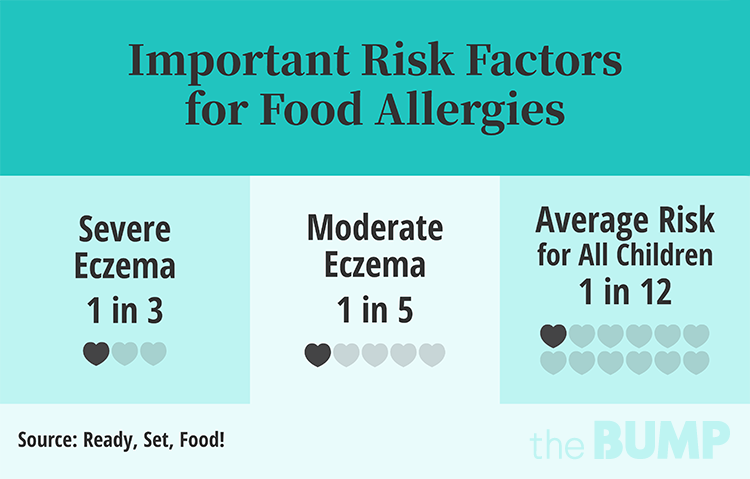
There are many factors that influence the development of food allergies in babies and children. However, these are the most common risk factors for children:
• Eczema: This is the most important risk factor for developing a food allergy. Eczema can increase your child’s food allergy risk by up to 8 times. The more severe the eczema, the greater the risk of food allergy. About one third of babies with severe atopic dermatitis will have a food allergy. Food allergies and eczema are strongly linked, as they are both part of what’s known as the “Atopic March,” a progression of related allergic conditions that tend to show symptoms in the following order: eczema, food allergy, allergic rhinitis and asthma. Interestingly, food allergy does not cause eczema, but the opposite is probably true. Of course, not every child that suffers from atopic dermatitis will develop all of these related conditions; however, research suggests that they’re strongly associated.
• Delayed introduction to allergens: Recent research shows that introducing baby to allergens early (starting at 4 months of age) and often can help prevent a food allergy. In fact, delaying allergen exposure can actually put your child at an increased risk for developing a food allergy. Introducing allergens starting at 4 to 6 months is recommended for every baby, especially for babies with eczema and/or a family history of food allergies.
The FDA has declared eight foods as the most common allergens in the US: egg, milk, peanut, shellfish, fish, soy, wheat and tree nuts. However, of those top eight allergens, peanut, egg and milk represent the most common food allergies in babies. Here’s what you need to know about each of these three:
Egg
- Affects 2 percent of children
- Usually presents in the first year of life
- About 85 percent of children “outgrow” (or become tolerant to) their egg allergy, which often happens as late as the teenage years
Milk
- The most common food allergy in babies and young children
- Affects 2 to 3 percent of children under 3 years old
- Usually presents in the first year of life
- Though most children outgrow their milk allergy, it remains the most common cause of reactions in school
Peanut
- Affects up to 2 percent of children
- Peanut allergy is more likely to be lifelong; only 20 percent outgrow a peanut allergy
- Although peanut is the allergen most often associated with severe or fatal reactions, any food allergen has the potential to cause anaphylaxis
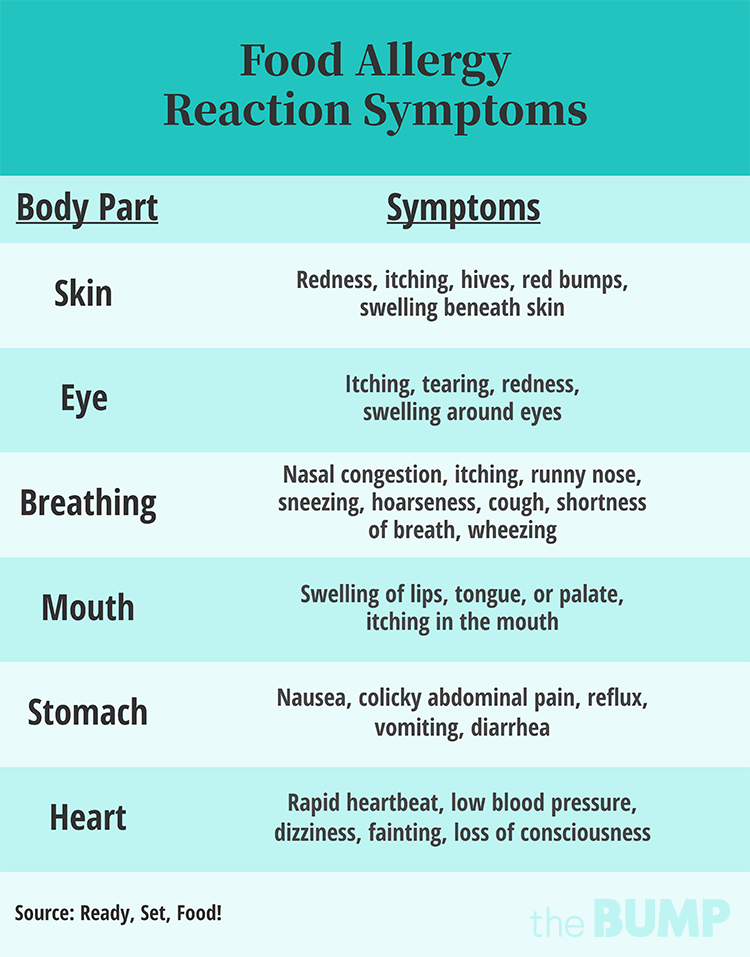
The most common symptoms of a food allergic reaction are hives, swollen lips and/or tongue, stomach upset and breathing problems. Hives and vomiting are the most common baby food allergy symptoms, which range from mild to severe.
Signs of a mild food allergy reaction include:
- Localized Hives
- One or two episodes of vomiting
- Itchy, watery eyes
- Runny nose
- Itching
- Local skin redness
These symptoms typically occur within two hours—and usually within minutes—after eating the allergy-causing food.
Symptoms of a severe food allergic reaction can include:
- Swelling of the tongue
- Swelling or tightness of the throat
- Difficulty breathing
- Noisy breathing
- Difficulty swallowing
- Persistent coughing
- Wheezing
- Difficulty vocalizing
- Persistent vomiting
- Change in voice or cry
- Pale appearance
- More than 50 percent of the body turning red
- Dizziness
- Fainting /collapse
- Feeling floppy (in infants and young children only)
- Progress of mild symptoms or two types of mild symptoms
When symptoms involve more than one organ system and are severe, it’s called anaphylaxis, which can be life-threatening and requires urgent medical attention.
Not every episode of hives, vomiting or runny nose is a sign of food allergy in baby. Many things can cause these reactions, including a virus or contact with other non-food allergens (like a dog, cat or pollen). Some foods just irritate the skin where it touches—known as a contact reaction—but don’t prompt any other concerns. When in doubt, stop offering the food and discuss with your child’s pediatrician.
If you do notice signs of a food allergy in baby, what to do next depends on how severe the baby food allergy symptoms are.
If baby has a mild or moderate reaction:
- Stop feeding baby the allergenic food immediately after noticing symptoms
- Carefully monitor baby for any other signs of an allergic reaction (remember, anaphylaxis is classified as symptoms involving more than one organ system and can be life-threatening)
- If symptoms progress or don’t improve, head to the emergency room
- Consult your child’s doctor as soon as possible
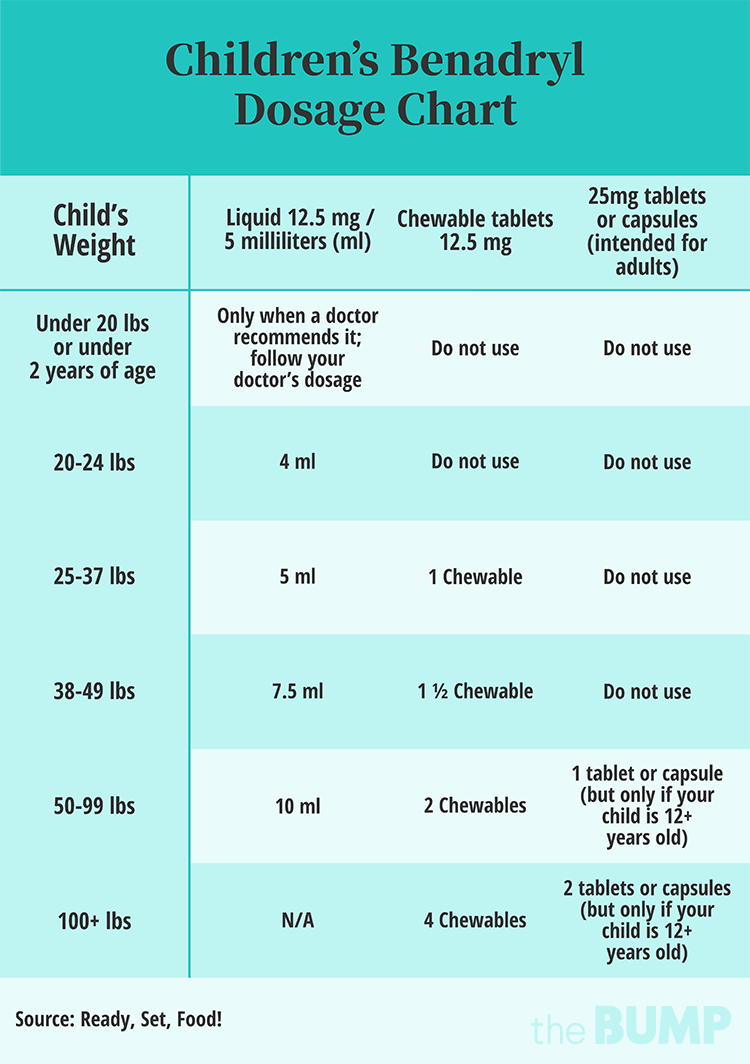
- With a doctor’s recommendation, you can give baby a children’s antihistamine such as Zyrtec or Benadryl
If baby has a severe reaction or anaphylaxis:
- Call 911 right away; let the 911 operator know that your child is having an anaphylactic reaction and ask for an ambulance
- Stop feeding baby the allergenic food immediately after noticing symptoms
- Lay baby flat in your arms; do not hold them upright or let them stand or walk
- If baby has fainted or is vomiting, lay them on their side
- If you have an epinephrine auto-injector (for example, Epi-pen or Auvi-q), administer according to the manufacturer instructions
Diagnosing food allergies in babies
If your child has a reaction that you’re concerned about, speak to your pediatrician or go to urgent care. They may refer you to an allergist for testing.
Most of the time, you can still keep breastfeeding baby even if they have a food allergy. In some instances, though, proteins from the allergic foods that naturally make their way into your breast milk can cause a reaction in baby. Food proteins can show up in breast milk anywhere between three to six hours after eating that food. If you’ve spotted signs of a food allergy in baby, or have any concerns, discuss with your doctor if you should remove anything from your diet.
Recent research shows that food allergies in babies can be prevented through early and consistent introduction of allergenic foods. In fact, USDA dietary guidelines recommend introducing infants to potentially allergenic foods starting at 4 to 6 months of age.
The American Academy of Allergy, Asthma, and Immunology (AAAAI), along with other leading medical organizations, has published guidelines with recommendations for how to go about introducing allergens into baby’s diet.
According to the AAAAAI, once a number of solid foods have been introduced and peanut-containing foods are eaten without any reaction, you can start to introduce other allergens. A common recommendation is to offer new allergens one at a time over a three-day period; discuss with your child’s pediatrician what approach will be best for your baby. There’s no specific order that other allergens should be introduced or wait time between new foods.
Introducing peanut
It’s recommended to feed baby 2g of peanut protein three times a week—but whole, shelled peanuts and lumps of peanut butter can pose a choking hazard for babies. Instead, you can offer:
- 17g of peanut puffs (e.g., Bamba or Cheeky Monkey)
- 9-10g of smooth peanut butter, mixed with hot water and then cooled
- 8g of ground peanuts
- 4g defatted peanut flour (eg, PB2 powder or PB fit)
These doses are approximate targets to aim for. Keep in mind, per the AAAAI, “we just don’t know if smaller amounts or less frequent feeds will be as protective against the development of peanut allergy.”
Introducing eggs
The AAAAI recommends offering baby fully cooked eggs to start with; this can be in the form of hard boiled eggs, baked goods like muffins, or pancakes containing egg. Undercooked eggs aren’t advised for babies under one year old.
Introducing milk
If you haven’t given baby any infant formula (which is typically milk-based), start introducing milk through baked foods or yogurt (plain, full-fat yogurt is best). You can begin giving baby cheese around 6 or 7 months.
Introducing soy
You can offer baby soy milk, soy yogurt or tofu. Soy milk can be added to baby’s bottle, and tofu can be blended with baby oatmeal or rice cereal. Avoid giving soy sauce, as it contains very little soy protein but a lot of salt.
Introducing fish and shellfish
Fish and shellfish are not major childhood food allergens, so it’s not as important to feed them to babies. Plus, there are way too many varieties of fish and shellfish out there to give baby a taste of all of them. The best approach is to simply offer the seafood that you tend to eat as a family and continue with regular intake. If baby isn’t ready for finger food yet, you can puree the fish, or just wait until baby is older.
Introducing wheat
Softly cooked pasta makes for great finger food. And in addition to containing eggs, pancakes and muffins can be a good way to introduce wheat.
Unfortunately, many parents struggle with feeding so many different allergens to babies. For example, in the biggest clinical trial on food allergy prevention, over 50 percent of families were not able to feed allergens to their baby early and often enough to prevent food allergies.
To help families with the challenges of early food introduction, there are products on the market to help make it easier for parents to feed allergenic foods to babies. Look for a product that you’ll find easy to use, that follows the amounts of each allergen used in clinical trials and allows you to start feeding top allergens like peanut and egg one at a time. While introducing allergens at 4 months can be effective for many parents, there are a lot of babies who aren’t ready to regularly eat solids at that age. One company, Ready, Set, Food!, has put allergens like peanut and egg into a powder that dissolves in breast milk or formula to suit those babies who are not yet reliable eaters.
However you go about it, the most important thing is that you start feeding allergens to baby early and often, starting at 4 months of age. Whatever method works for you, just do it.
About the expert:
Jonathan M. Spergel, MD, received his medical and graduate education at the Mount Sinai School of Medicine in New York City and completed his pediatric residency at Yale-New Haven Hospital in New Haven, Connecticut. His clinical and post-graduate research training in allergy and immunology were completed at Children’s Hospital, Harvard Medical School in Boston. Spergel is board-certified in pediatrics as well as allergy and immunology. He is currently chief of the allergy section at The Children’s Hospital of Philadelphia, Perelman School of Medicine at the University of Pennsylvania, as well as a member of the scientific advisory board for Ready, Set, Food!, a complete guided system for early allergen introduction.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.