What a Septate Uterus Might Mean for Your Pregnancy
The journey to becoming a parent will look different for everyone, and it can be far from easy. One thing that may affect your efforts to conceive? A septate uterus. While this birth defect is rare, it can be one of the most common ones to affect the uterus. We asked experts to break down everything to know about what a uterine septum is, what causes it and how it may affect your pregnancy journey.
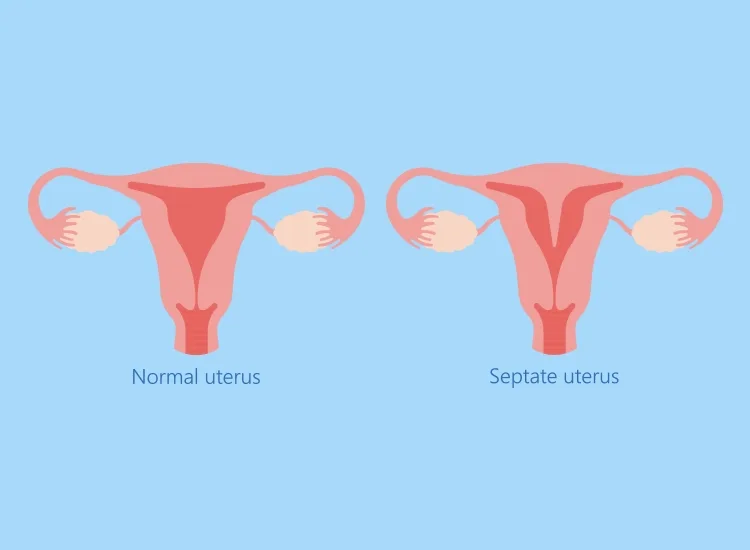
A septate uterus, also referred to as a uterine septum, is a birth defect women can have from their own time in the womb, says Lucky Sekhon, MD, an infertility specialist and ob-gyn at RMA of New York. During a female’s fetal development, there are two ducts—called Müllerian ducts—within the uterus that are supposed to join together and absorb the connecting fiber and tissue. However, if this merger fails to happen correctly, some of the tissue can remain and form a septum, Sekhon explains, which is a wall of fibrous tissue that divides the uterus into two halves. It usually runs down the middle of the uterus and can vary in its length and thickness, says Sherry Ross, MD, an ob-gyn and women’s health expert.
How common is a septate uterus?
A septate uterus is a birth defect, which means that all women who have one are born with it. “It’s one of the more common uterine anomalies, accounting for up to 90 percent of these [types of] birth defects,” Ross says. However, overall, only 4 percent of women have a uterine septum, adds Sekhon.
There are two types of uterine septum: complete and partial. The type you have will depend on how far the septum extends down your uterus.
-
Complete septate uterus: A complete septate uterus occurs when there’s a membrane that runs from the top of the uterus and extends down to the cervix (or, in rare cases, into the vagina), Ross explains. Essentially, in a complete septate uterus, the septum divides the entire uterus into two separate compartments.
-
Partial septate uterus: A partial septate uterus occurs when the septum only partially extends into the uterus, rather than fully dividing the uterus into two, Sekhon says. A partial septate uterus usually doesn’t affect the cervix or the vagina.
According to Ross, some people go on to have an uncomplicated and successful pregnancy with a septate uterus, depending on the type and size of the septum. However, pregnancy with a septate uterus can also come with an increased risk of complications such as:
- Preterm labor
- Abnormal fetal position (such as breech or transverse lie)
- Low birth weight
- Increased risk for a c-section delivery
A septate uterus in pregnancy may also increase the risk of miscarriage. The septum has “little to no blood supply—and presents added surface area for implantation of an embryo,” Sekhon explains. “If an embryo implants in the septum, there is a high risk of miscarriage.”
Unfortunately, there aren’t really many uterine septum symptoms to watch for. Some subtle signs may include painful menstruation and menstrual cramps, but for the most part the condition is asymptomatic. “Many people with a septate uterus are unaware of their birth defect until they try to become pregnant,” Ross says. Recurrent miscarriages while trying to conceive could be another sign of a septate uterus, Ross adds.
Because the condition is asymptomatic, it’s usually best diagnosed through visual tests and imaging that allow the physician to see the “inner and outer contour of the uterus,” Sekhon explains, such as a 3D pelvic ultrasound or MRI. “This allows for clearly distinguishing between a septum and [another type of uterine irregularity like] a bicornuate uterus.”
The good news? Uterine septums are treatable. “Depending on the size and disruption of the uterine membrane, a septate uterus can be managed without any surgical intervention,” Ross says. However, if the septum is significant, a uterine hysteroscopy might be performed to remove it.
“A hysteroscopy involves using a long thin camera, which is passed through the cervix into the uterine cavity to visualize the septum and either side of the cavity,” Sekhon explains. Having good visualization during the uterine septum hysteroscopy plays a key role in its success. If your physician needs more help seeing the septum, they may use inflated balloons to help the tube reorient or fluids to expand the uterus. Once they have good visualization, “a loop, scissors or other tools can then be used to incise the fibrous septum, which then allows the cavity to open up and become one whole cavity,” Sekhon explains.
Uterine septum surgery is minimally invasive and usually takes between 30 to 60 minutes, Sekhon says. In fact, most patients are sent home the same day. Plus, it’s typically covered by insurance, Ross adds. (But, if it isn’t, the hysteroscopy may cost between $2,000 and $4,000.)
Uterine septum hysteroscopies are usually highly successful, both Ross and Sekhon say, since once the septum has been removed, it can’t grow back. Pregnancy and reduced miscarriage rates following treatment for a septate uterus can be as high as 65 percent, Ross adds. However, as is true with any medical procedure, uterine hysteroscopies do have some risks. According to both experts, these can include:
- Abnormal bleeding
- Infection
- Postoperative adhesions inside the uterus
- A failed procedure due to lack of adequate visualization of the septum
- Damage to the cervix
- Uterine rupture during future pregnancies
- Perforation of the uterus (and a low chance of damage to the organs surrounding the uterus)
- Fluid overload (the fluid may be used to expand the uterus) from the hysteroscopy
While these sound scary, know that—because the procedure is usually so quick—the risk of fluid overload is very unlikely, Sekhon says. Similarly, the risk of perforation is also low—less than 5 percent, she adds.
Your risk level depends on your individual factors, such as your surgeon’s experience, how well they’re able to see the septum and the difficulty level of your case (whether the septum is complete or partial). “If a case is challenging, the hysteroscopy can be done under laparoscopic guidance to better guide where the camera is on the inside of the cavity,” Sekhon explains. “Sometimes you can see the light from the hysteroscopy on the outside of the uterus and determine which part of the cavity you are in to get your bearings. Damage to the cervix or uterus is rare, but of course any time a uterine procedure is done the risk of perforation must be discussed.” Remember, when assessing any risks and factors, it’s always best to consult with your doctor on the best options for you based on your individual circumstances.
Pregnancy after uterine septum removal
The good news is that the procedure to treat a septate uterus is fairly straightforward, so patients don’t have to wait too long afterward to start trying again. Doctors typically ask patients to wait at least two months before trying to conceive again to give the endometrium time to heal. Always consult with your doctor on how long to wait following septate uterus treatment for your specific circumstances.
The bottom line? A septate uterus is a birth defect that can often go undetected until a woman starts trying for a baby. While a healthy pregnancy is possible, take heart in knowing treatment for a septate uterus is achievable and often highly successful. “The vast majority of women can go on to have a healthy pregnancy,” Ross says. For questions about your situation, don’t hesitate to reach out to a provider you trust. They’ll be able to best answer your questions and help you navigate your individual path to baby.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from the Bump:
Sherry Ross, MD, is an ob-gyn, women’s sexual health expert and author of She-ology: The Definitive Guide to Women’s Intimate Health. Period.(https://www.amazon.com/dp/B06XNTBL4Z?&linkCode=ll1&tag=tb-septate-uterus-20&linkId=5ccbefa112134c16b786f03daa0e1fd5&language=en_US&ref=asli_ss_tl) and She-ology, The She-quel(https://www.amazon.com/gp/product/B08299DLBR?&linkCode=ll1&tag=tb-septate-uterus-20&linkId=b5d0c9e6dd1fab631f8b582bd8cd3a55&language=en_US&ref=asli_ss_tl). She earned her medical degree from New York Medical College.
Lucky Sekhon, MD, is an infertility specialist, reproductive endocrinologist and ob-gyn at RMA of New York. She’s also an assistant clinical professor at the Icahn School of Medicine at Mount Sinai and a fellow in the American College of Obstetrics and Gynecology. She received her medical degree from the Royal College of Surgeons with the University of Dublin in Ireland and completed her residency at the Icahn School of Medicine at Mount Sinai in New York City.
Learn how we ensure the accuracy of our content through our editorial and medical review process.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.