How a Psychiatric Nurse Dealt With Her Own Prenatal Depression
I glanced down at my swollen belly and released a heavy sigh. The baby had transformed from a gentle butterfly, fluttering deep in my stomach, to a Bruce Lee wannabe, delivering roundhouse kicks to my bladder. A distinct knee then forearm rose and rolled the perimeter of my abdomen before pausing to thrust a one-two punch into my ribcage. I couldn’t help but think of the chest-bursting scene from Alien.
Sigourney. Help.
Jokes aside, I was beginning to seriously wonder if I needed help. After wrestling two little boys to bed, I could hardly get to my room before collapsing in a heap of hopelessness anxiety and heaving sobs.
I never expected to be one of the 14 to 23 percent of women experiencing prenatal depression.
And I most certainly never expected that sad, achy night to churn out thoughts of worthlessness and self-harm that had me dialing the first help number my search engine spit out: a depression hotline—in Australia.
“Hallo, mate. You’ve reached the prenatal depression line. We are currently closed. If this is a crisis, please dial Australian emergency services to receive help…”
I slowly ended the call, realizing how very deep in this hole I was.
There were people and resources here in the US, not a few oceans and a continent away, that could help me return to normal or even better. I had a husband eager to jump in and support me, but I was unwilling or unable to talk to him about how I was feeling.
Meditation, therapists, medications and relationship tools like Lasting (powered by The Bump parent company) are all incredibly helpful when you find yourself unable to keep the tears at bay, wondering how in the world you got here.
You got here because prenatal depression is still depression. Chemicals in your brain that regulate emotion and feelings become imbalanced, causing a myriad of problems. It can happen slowly, subtly taking root over time, or it can occur quickly through trigger situations (i.e., job loss, relational conflict, childhood trauma or even extended sleep deprivation).
I was a psychiatric nurse before motherhood and sat countless times with tearful, exhausted, loss-consumed patients who looked around in confused disbelief at their hospital gowns as if they’d teleported there. I’d tell them they couldn’t do this alone, that depression was not a weakness but a disorder to be treated like heart disease or cancer, and they were in a safe place to receive care and help.
So if I knew all that, taught all that, believed all that, why was I unable to see I was in the throes of just a different type of depression that happens to strike during pregnancy? Julia Houdek, APNP, a Wisconsin-based ob-gyn nurse practitioner, talks about this obliviousness: “I see pregnant women come in all the time, saturated with depression, sleeplessness, suicidal thoughts and utter hopelessness,” she says. “They can’t see it in themselves because of the fast pace of life’s demands. I’m often the one to tell them, encourage them, to get on a treatment regime because there are serious consequences to both mother and baby when prenatal depression goes untreated.”
If you’re experiencing any of these signs consistently for two or more weeks, talk to your obstetrician:
• Hopelessness or helplessness. Life feels dim and you feel powerless to change anything so you don’t even try.
• Excessive sleep or insomnia. Both can be normal with pregnancy, but not if you’re sleeping most of the day or unable to get more than a few hours most nights, let your doctor know.
• Isolation or anxiousness. Consistently withdrawing from people and activities you enjoy and feeling on edge, agitated or panicky can be indicators of prenatal depression.
• Persistent, intrusive thoughts. For example, “What kind of mom will I be to this baby when I can’t even brush my hair?” or “They would all be better off without me; I’m such a mess,” are red flags.
• Thoughts of self-harm. They can be passive (“I just want to disappear. I don’t want to be here anymore) or active (“I want to drive into a wall”); either way, they indicate a very serious progression of depression and call for immediate intervention.
If you find yourself feeling this way, you need to get help—and that can come in many forms.
• Tell someone. Don’t hide this a minute longer. Pick up that phone, call your husband, partner, best friend, neighbor or hotline. The number for the National Suicide Prevention Lifeline is 1-800-273-8255.
• Counseling. In person, one-on-one sessions with a trained, professional guide can provide tremendous benefit.
• Medication. There are several medications that have been proven safe and effective during pregnancy. The potential risks of uncontrolled anxiety and depression frequently outweigh the theoretical risks of needed medications.
• Relationship counseling. The Lasting app is a relational counseling tool that can be accessed right from your phone. It’s a valuable resource for helping your partner identify your needs and care for you through the sadness of this season. For example, its sex series points to research showing that 15-minute daily massages can lead to lower stress and depression during the postpartum period.
Although friends and family may be eager to help, prenatal depression calls for more than a good night’s sleep, a vent-fest to a friend or even Sigourney Weaver’s alien-blasting skills. So call your doctor, talk to your partner or support system and download Lasting. It’s what helped me through my own prenatal depression. You may feel a thousand miles from happy, but help is closer than you think.
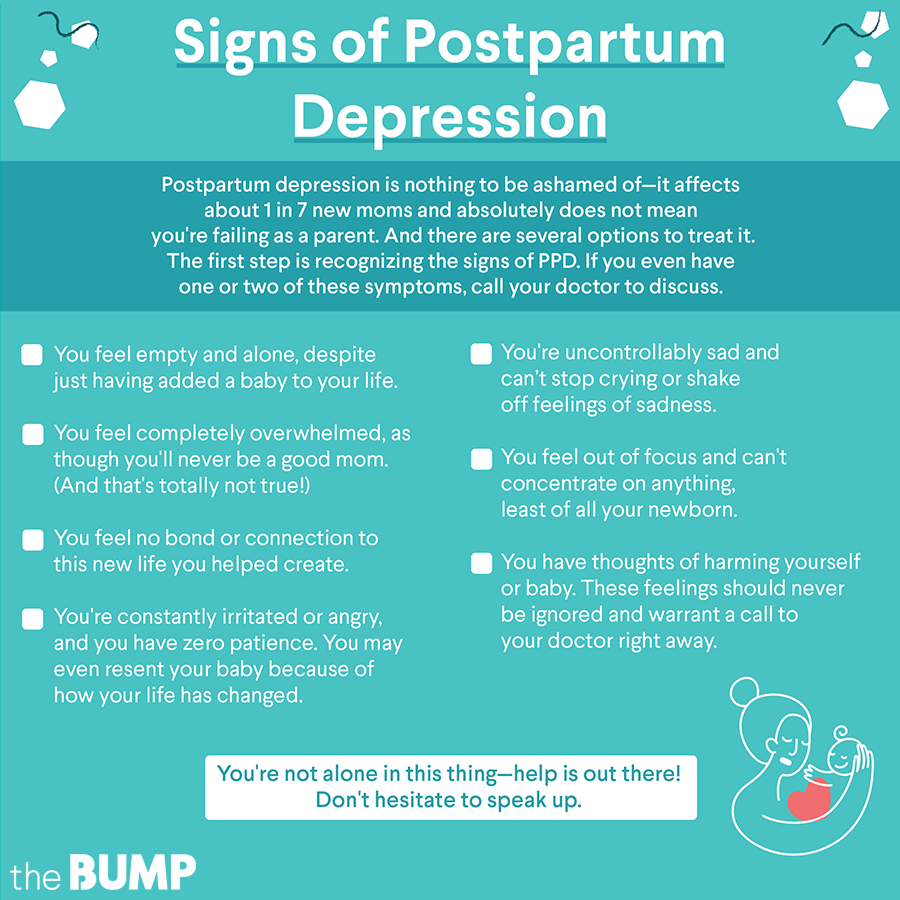
Review signs of postpartum depression here:
Cassidy Doolittle is a psychiatric nurse turned stay-at-home mom who lives with her family in Texas.
Published February 2019
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.