Epidural 101: How It Works
Labor and delivery is stressful no matter how you cut it, so having a basic birth plan in place can help you feel some semblance of control. To that end, you’ll want to explore your options and know what to anticipate when it comes to getting an epidural (or not). Ready to find out everything you’ve ever wanted to know about the ultimate numbing needle? We’re sharing answers to all your top questions: How long does an epidural last? Does getting an epidural hurt? And what are epidural side effects? Read on to get the facts.
You know those screaming women in labor you’ve seen in movies and on TV? Chances are they didn’t have an epidural. Simply put, an epidural helps to ease the pain of contractions and delivery. Numbing medication is sent to the area around your spinal cord (called the epidural space) via a catheter tube, and “this makes you numb from the belly button down,” explains Erin S. Grawe, MD, an assistant professor of clinical anesthesiology and director of perioperative services at the University of Cincinnati College of Medicine. Numb, yes, but not sleepy, which means you’ll be alert and at ease throughout baby’s delivery.
There are a few different types of epidurals that offer varying degrees of pain relief:
- Standard epidural. A “regular” epidural injects anesthetics into the epidural space of your spine to block pain in your body, making you numb from the waist down. It blocks your motor control, so while you’ll be able to move your legs around in bed, you won’t be able to walk with a full epidural, says Christine Greves, MD, an ob-gyn at the Winnie Palmer Hospital for Women & Babies in Orlando, Florida.
- Spinal injection. This one-and-done shot sends a single dose of concentrated drugs into the spine’s sac of cerebrospinal fluid, which houses the spinal cord and nerves. It provides immediate relief, but because there isn’t a catheter or continuous flow of medication, this option wears off within about two hours. It’s often used for a C-section.
- Combined spinal-epidural. This combo can offer the best of both worlds: Like a spinal, the numbing medicine is injected into the fluid sac, so you’ll feel the effects quickly, and like an epidural, a catheter is then inserted to provide ongoing pain relief.
- Low-dose epidural. This option offers a lower dose of the pain-blocking medication, leaving you with greater movement in your legs. It’s often administered in the early stage of labor, Greves says, before pain levels spike.
- Walking epidural. A walking epidural uses narcotics only to help lessen the pain without limiting your motor function. It won’t block the pain as much as a standard or low-dose epidural, Greves says, but you may be able to get up and walk around during labor, if your doctor and hospital allow it.
If you opt for a walking or low-dose epidural to begin with but decide you need more pain relief, you can upgrade your epidural as you go—but you can’t downgrade from a standard epidural to a low-dose option, or from a low-dose epidural to a walking one.
What is in an epidural?
Wondering what’s in an epidural? Usually they include local anesthetics (or numbing medicine) and a narcotic (or pain-relieving medicine), explains Rebekah Mustaleski, CPM-TN, a certified professional midwife and compression director with Motif Medical, as well as preservatives and stabilizers. “Adrenaline is also usually included to extend the effectiveness of the epidural,” she adds. Rest assured all experts and medical professionals say that epidurals—and their ingredients—are usually safe for mom and baby (more on this below).
Technically, you can get an epidural at any time during labor, but it’s often recommended that you do so during the active phase (i.e., the middle stage when your cervix begins to dilate rapidly), says Greves. That’s because an epidural could actually slow down labor, she says, so it’s best to administer it when things are already progressing quickly.
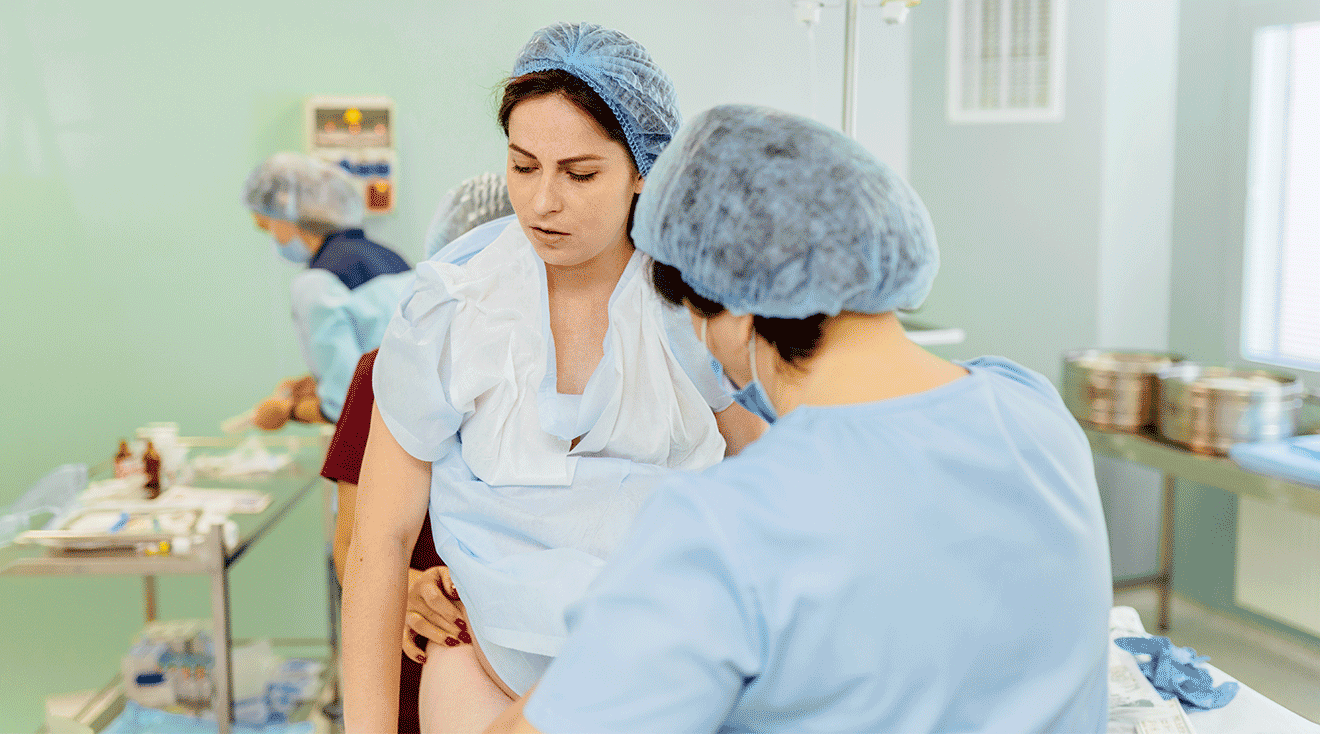
While you might be tempted to wait until you’re in teeth-clenching, unbearable pain to get an epidural, it’s actually better to do it before you reach the writhing point. A woman must be able to sit still when an epidural is administered, says Grawe—otherwise, it may be difficult for your anesthesiologist to safely give you one.
Here’s what they didn’t teach you in biology class: Epidural medication is delivered through a tiny, flexible tube (aka a catheter) that’s inserted into your lower back. The tube goes into the epidural space, which is outside of the spinal cord and where all of the nerves live that go to the lower parts of the body, Grawe says. Doctors use the tube to administer special medication—often a combo of a local anesthetic and a narcotic—near those nerves. “The medication basically dazes the nerves, so you don’t feel the pain impulses coming in,” says William Camann, MD, director of obstetric anesthesia service at Brigham and Women’s Hospital in Boston and coauthor of Easy Labor: Every Woman’s Guide to Choosing Less Pain and More Joy During Childbirth.
Don’t worry if you’re planning on getting an epidural early in labor; the pain medication won’t suddenly stop working or wear off. The epidural stays in your back so you can continue to receive the medicine throughout labor. And here’s some comforting news: Many hospitals now have patient-controlled epidurals, which allow moms-to-be to manage the flow of pain-relieving epidural medication with the simple push of a button. But don’t worry: The machine is set so that it won’t deliver too much medication.
So how long does an epidural last? An epidural can provide relief for a pretty long time, as long as your catheter is in place and you’re receiving medication—in fact, it can last reliably for up to five days, according to Grawe. “Fortunately, labor doesn’t usually take that long, so the epidural doesn’t need to last that long,” she points out.
Some doctors will request that the epidural be turned off or down during the pushing phase to allow mom to feel the pressure of baby’s head, which creates an urge to push, says G. Thomas Ruiz, MD, an ob-gyn at Orange Coast Memorial Medical Center in Fountain Valley, California. But that can still make things tricky: “Turn down the epidural too soon and the pain of contractions can inhibit pushing in some women,” Ruiz says.
Once baby is delivered, your anesthesiologist will stop the medicine and pull out the catheter. After that, Grawe says, it can take up to four hours for the numbness to wear off.
While getting an epidural is meant to reduce labor pains, many women worry and wonder: Does getting an epidural hurt? The good news is the actual process of receiving an epidural is often not as scary—or painful—as you might imagine.
Everyone’s pain tolerance is different, Greves says, but in general, it’s not painful—and definitely not nearly as uncomfortable as active labor pains. In fact, your anesthesia provider will help ensure you’re at ease by numbing the skin on your back with a small needle even before actually placing the epidural, Grawe says. “After that, you may feel pressure and pushing in your lower back, but nothing should feel like sharp pain,” she says. If you do feel anything sharp, just let your anesthesiologist know and they can give you more numbing medicine, Grawe says. “The job of the anesthesia provider is to make sure you’re comfortable and safe during your delivery.”
How long is an epidural needle?
Still, some women are wary about getting an epidural because they’re nervous about the size of the needle. Depending on the kind of epidural you receive, it will likely be 3.5 inches long and a bit wider than an average shot. Not a fan of needles? Don’t worry—since the epidural is placed in your back, you’ll be facing away from the anesthesia provider and won’t have to see that needle at all.
Will you feel any pain after an epidural?
An epidural numbs the pain of childbirth, but it’s important that you’re still able to feel the urge to push. Many women report feeling pressure and a decreased sensation of pain during their labor. Overall, an epidural can provide a more comfortable experience and give you some much-needed relief. (You might even be at ease enough to take a nap! After all, labor can be long and exhausting.)
Of course, it’s worth noting that epidurals aren’t always 100 percent effective. According to a report in Anesthesiology, 10 to 15 percent of women experience incomplete pain relief or localized pain. If this happens, your anesthesiologist may withdraw and replace the catheter or offer additional doses.
If you’re considering getting an epidural, you may be concerned with safety and wondering: Does an epidural affect baby? In a nutshell, don’t lose sleep at night worrying whether an epidural will cause harm to you or baby. “Epidurals are very safe,” Grawe says, “and there are no negative effects on the fetus or the labor process when used appropriately and in a carefully monitored setting.” It’s true that trace amounts of the epidural can pass through the placenta to baby, Mustaleski notes, but this amount is usually too low to really affect baby in any way. (She does caveat, however, that changes in blood pressure due to an epidural may affect baby—more on this side effect below).
Overall, epidural complication rates are low: According to the American Society of Anesthesiologists, it’s just under 3 percent.
Epidurals are the gold standard in labor pain management, and they’re considered very safe. But there are some potential side effects. Women may have soreness in their lower back where the epidural needle was inserted, Greves says. There’s also a risk of developing what’s called a spinal or epidural headache—a headache that occurs if there’s a leak of spinal fluid around the epidural catheter. But it’s very rare, Grawe says, and only happens between 0.5 to 5 percent of the time. A woman might also have an infection at the site of the catheter, and bleeding or bruising in the epidural space, which can cause nerve damage—but again, Grawe says, this is extremely rare.
Other potential epidural side effects include:
- Drop in blood pressure. According to research, about 14 percent of women experience hypotension, or a sudden drop in blood pressure, after receiving an epidural. This drop in blood pressure may affect baby’s heart rate and make them sleepy after birth, Mustaleski notes. Your medical team will give you IV fluids, monitor your blood pressure and provide additional treatment, as needed.
- Nausea and vomiting. The opioids in an epidural may also make you feel drowsy and nauseous.
- Itchy skin. Opioids may also make you itchy and restless. If this happens, your doctor can give you medication.
- Fever. It’s possible to spike a fever after receiving an epidural.
- Labored breathing. It’s not common, but occasionally an epidural can cause slow or labored breathing.
- Problems urinating. Since your lower body will be numb from an epidural, you won’t feel the urge to pee and will likely have a urination catheter in place. It’s removed shortly after delivery, but there’s a chance you may continue to experience decreased bladder sensitivity for a short while.
- Trouble walking. Once the epidural wears off, you’ll start to regain strength in your lower body. However, it might take you a bit to feel fully steady on your feet.
- Nerve damage. It’s extremely rare, but it’s possible that an epidural could reach a nerve and cause temporary or long-term numbness.
Unfortunately, not all women are good candidates for an epidural. Your doctor will assess you to determine if it’s the right pain-management path for you. The following are among the more common reasons you may not be able to receive an epidural during labor:
- Very low blood pressure
- Some bleeding or clotting disorders
- Blood infections
- Skin infection or a brand new tattoo on the lower area of your back
Also, keep in mind that your birth plan may not be conducive to an epidural. For example, if you want to have a water birth or plan on delivering in your home or at a birthing center, you’re out of luck. You need to be in a hospital setting to get an epidural.
The choice to get an epidural during childbirth is an entirely personal one. Consider your pain tolerance, and discuss your birth plan with your provider. Be sure to ask about the different kinds of pain-management and epidural options available at your hospital and any restrictions that may apply. Above all else, try to be flexible and keep an open mind—because your birth plan can change on a dime. Epidural or no epidural, keep your eye on the prize: a healthy, happy and safe delivery.
Frequently Asked Questions
Do epidurals wear off?
According to Mustaleski, while everyone’s metabolism will process the epidural at different rates, most people tend to get full feeling back in their body between four and six hours after the epidural was discontinued.
How long after getting an epidural does baby come?
Unfortunately, this will be subjective, as it really depends on when during the birth process the epidural was administered. “The earlier you’re in the labor process when you get an epidural, the longer it will be before you give birth,” Mustaleski explains. For those wishing to deliver vaginally, she recommends waiting until you’re at least 6 centimeters dilated before getting an epidural. “Movement and gravity help your body to progress through early labor and your ability to change positions will be limited after you get an epidural,” she explains.
Can you feel baby coming out with an epidural?
As mentioned, most providers will want you to feel the pressure of baby’s head to encourage the need to push, so odds are you’ll feel baby coming out to some extent. However, like with all other things regarding pregnancy and childbirth, how well you’re able to feel baby coming out depends on your individual factors, such as how the epidural affected you and where it was placed. “In the end, some people can feel their baby coming out, even if they have an epidural. Other people don’t feel it,” Mustaleski says. Unfortunately, there’s no way to predict which camp you might be in.
What are the best labor positions with an epidural?
While there’s no “best” labor position, Mustaleski does cite movement as a beneficial factor. She suggests using pillows or a peanut ball to switch sides or the positioning of your legs every half hour to help labor progression.
Can an epidural work only on one side?
Again, how you feel the epidural will depend on its placement. “If you have anatomic variations, if the catheter is more to one side of the epidural space or if you only lay on one side after administration, then the medication may only affect one side of the body,” Mustaleski explains. Ideally, following epidural administration, try switching sides every 20 to 30 minutes to keep the medication moving through both sides of the body.
Can you get an epidural with a multiples pregnancy?
Not only can you get an epidural with a multiples pregnancy, but some providers may actually recommend it during labor, just in case the need for an emergency C-section arises, Mustaleski notes.
Can you get an epidural with a tattoo?
While it’s possible to get an epidural with a tattoo, Mustaleski says that ultimately it’ll be up to the discretion of the anesthesiologist. They may want to find a spot free of ink to place the epidural, particularly if the tattoo is new and still healing.
Can you get an epidural if you have back problems?
For people with back injuries or a history of back issues, such as scoliosis, an epidural may not be advised during childbirth, Mustaleski says. “If you’re concerned about your situation, it’s best to talk about this in advance with your care provider.”
The choice to get an epidural is ultimately personal and each individual’s circumstances will vary. Chat with your provider and prenatal care team about their recommendations and the best options for you and baby.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
William Camann, MD, is an associate professor at Harvard Medical School and the director of obstetric anesthesia service at Brigham and Women’s Hospital in Boston, Massachusetts. He received his medical degree at Pennsylvania State University College of Medicine in Hershey, Pennsylvania.
Erin S. Grawe, MD, is an assistant professor of clinical anesthesiology and director of perioperative services at the University of Cincinnati College of Medicine in Cincinnati, Ohio. She also received her medical degree there.
Christine Greves, MD, is an ob-gyn at the Winnie Palmer Hospital for Women & Babies in Orlando, Florida. She earned her medical degree from the University of South Florida College of Medicine in Tampa, Florida.
Rebekah Mustaleski, CPM-TN, IBCLC, is a certified professional midwife specializing in evidence-based maternity care. She co-founded Roots & Wings Midwifery in Knoxville, Tennessee. Mustaleski received her bachelor’s degree in psychology from Centre College and worked as a doula and birth photographer prior to establishing Roots & Wings.
G. Thomas Ruiz, MD, is an ob-gyn at Orange Coast Memorial Medical Center in Fountain Valley, California. He received his medical degree from UC Irvine School of Medicine in Irvine, California.
Anesthesiology, Treatment of Incomplete Analgesia after Placement of an Epidural Catheter and Administration of Local Anesthetic for Women in Labor, June 1998
American Society of Anesthesiologists, Large study delivers message to expectant mothers: Epidural, spinal anesthesia safe choices for relieving pain, October 2014
Institute for Quality and Efficiency in Health Care, Birth: Learn More – Epidurals and other medications to relieve labor pain, October 2022
Learn how we ensure the accuracy of our content through our editorial and medical review process.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.