What Is an Ectopic Pregnancy?
After that positive test result, you start dreaming of life with baby, and you hope that everything goes swimmingly throughout the nine-month journey ahead. Unfortunately, unexpected complications can arise. One relatively uncommon but nevertheless plausible issue is an ectopic pregnancy.
Sometimes referred to as a tubal pregnancy, an ectopic pregnancy is never a viable one—meaning, it won’t result in a baby. Moreover, it can be incredibly dangerous or even fatal if left untreated. So what are the signs of ectopic pregnancy, and how is it diagnosed and treated? Read on for expert intel.
An ectopic pregnancy happens when a fertilized egg grows outside of the uterus, explains Christine Greves, MD, a board-certified ob-gyn at the Winnie Palmer Hospital for Women and Babies in Orlando. “It’s a pregnancy where a pregnancy should not be,” she adds.
An ectopic pregnancy most often forms in the fallopian tube, which is where a sperm and an egg meet to create a pregnancy, says Anastasia Matthews, MD, an ob-gyn at the Ohio State University Wexner Medical Center. “Ectopic pregnancies can be dangerous because the pregnancy is growing in a confined space and can rupture if left untreated, which leads to bleeding within the abdomen.” This can become a life-threatening medical emergency, emphasizes Greves, reiterating that an ectopic pregnancy will never be a viable pregnancy: “It’s incompatible with having a baby at the end.”
According to the Cleveland Clinic, ectopic pregnancies occur in about 2 percent of all pregnancies.
Anyone can experience an ectopic pregnancy: The American College of Obstetricians and Gynecologists (ACOG) points out that about 50 percent of people who have an ectopic pregnancy have no known risk factors. However, there are some elements that can raise your chances of experiencing one.
What are ectopic pregnancy risk factors?
Per ACOG, ectopic pregnancy risk factors include:
- A previous ectopic pregnancy
- Prior fallopian tube surgery
- Previous pelvic or abdominal surgery
- Certain sexually transmitted infections (STIs)
- Pelvic inflammatory disease
- Endometriosis
- A history of infertility
- Using assisted reproductive technology like IVF
- Being older than 35
- Smoking cigarettes
There are a few signs that you may be experiencing an ectopic pregnancy, says Meleen Chuang, MD, interim chief of service of ob-gyn at NYU Langone Hospital, Brooklyn. Ectopic pregnancy symptoms include:
- Pain on one side
- Severe abdominal pain
- Abdominal swelling
- Dizziness
- Chest pain
- Shortness of breath
Rest assured that these symptoms don’t always point to a serious complication like an ectopic pregnancy. That said, it’s important to talk to your ob-gyn about anything out of the ordinary.
When do ectopic pregnancy symptoms start?
Wondering when the pain of ectopic pregnancy starts? “Symptoms can start [early on], much like how spotting and cramping can be present at the beginning of a normal pregnancy within the uterus,” Matthews says. “However, the pain of an ectopic pregnancy doesn’t resolve on its own and will progressively get worse.” Ultimately, though, when it comes to ectopic pregnancy symptoms, there’s no definitive timeline for when they’ll kick in.
What does an ectopic pregnancy feel like?
There’s some variability and subjectivity in terms of pain. If it’s early, Chuang says you may feel nothing at all. But as an ectopic pregnancy progresses, the discomfort becomes more pronounced and more intense. “The abdominal/pelvic pain can initially be a cramping-type pain, but typically the pain becomes more constant as the pregnancy grows,” Matthews says. “The pain is also usually located on one side of the body.”
Does your belly grow with an ectopic pregnancy?
During a typical pregnancy, your bump grows as your uterus gets bigger, Greves says. “The belly doesn’t grow with ectopic pregnancy because the pregnancy doesn’t have enough space to expand and grow normally in the fallopian tubes,” Chuang says.
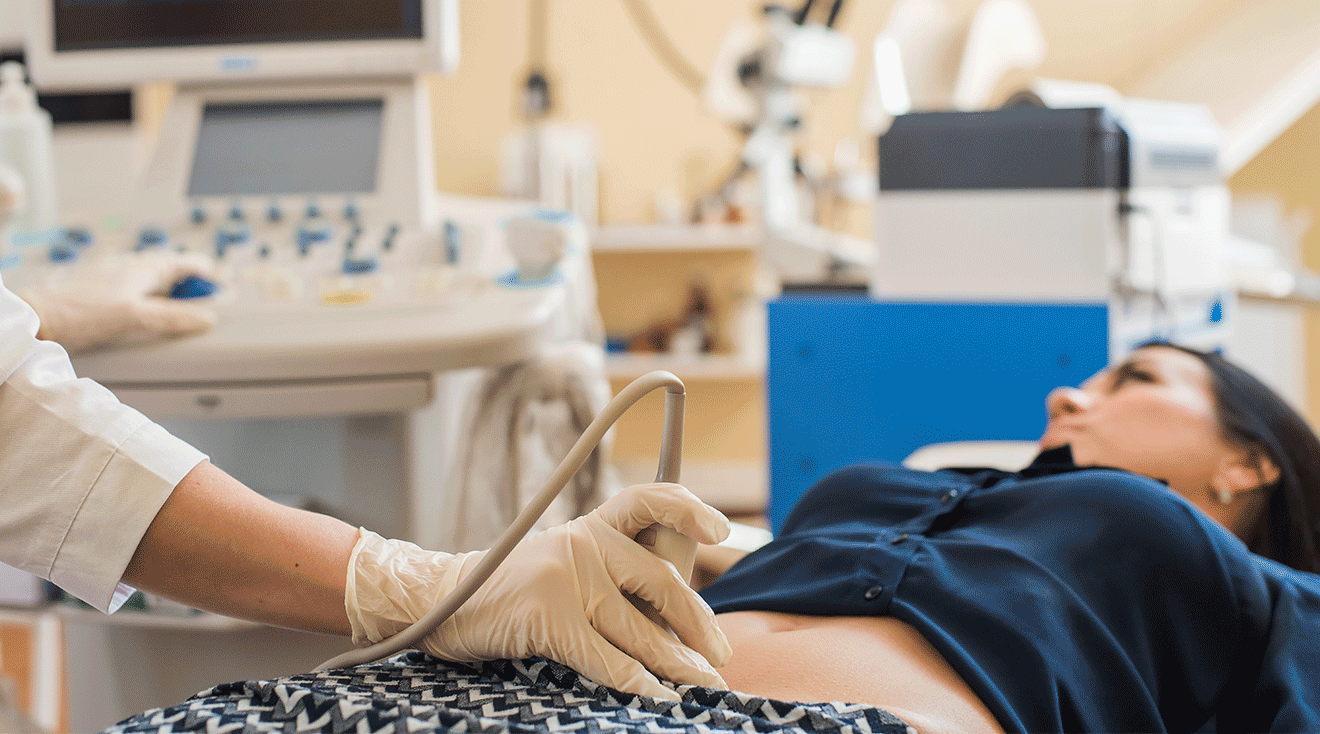
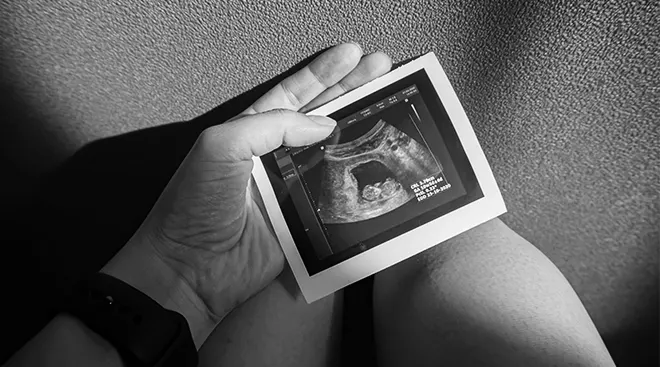
Ectopic pregnancy is usually diagnosed with an ultrasound and a bHCG test, which tests your blood for a pregnancy hormone called human chorionic gonadotropin (hCG), Matthews says. Ultimately, the ultrasound can determine if the pregnancy is in the uterus or not. “If you see an embryo or sac outside the uterus, that’s diagnostic,” Greves says
There are a few treatment options, and they largely depend on what stage your ectopic pregnancy was diagnosed. “If it’s caught early enough and not ruptured, treatment is with an injection called methotrexate,” Chuang says. “Methotrexate stops growth of fast-growing cells—pregnancy tissue is fast-growing cells.” In some situations, surgery may be needed to remove the ectopic pregnancy.
Unfortunately anyone can experience an ectopic pregnancy, whether they have risk factors for the condition or not. “There isn’t a way to prevent a pregnancy from being an ectopic pregnancy,” Matthews says. “However, quitting smoking and limiting unprotected intercourse when not trying to become pregnant—to avoid sexually transmitted infections—can mitigate some risk factors.”
Experiencing an ectopic pregnancy can be emotionally devastating. Moreover, it can potentially impact your fertility for some time, says Chuang. She adds that “thankfully, about 65 percent of women who’ve had this condition go on to have a healthy pregnancy within 18 months.”
A previous ectopic pregnancy also increases your risk of having one later on, but doctors stress that it doesn’t mean you can’t have a healthy pregnancy—and baby—in the future. “It’s absolutely still possible to have a normal intrauterine pregnancy after an ectopic pregnancy,” says Matthews. Talk to your doctor if you have any questions or concerns about getting pregnant again after an ectopic pregnancy.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Christine Greves, MD, is a board-certified ob-gyn at the Winnie Palmer Hospital for Women and Babies in Orlando. She earned her medical degree from the University of South Florida College of Medicine.
Meleen Chuang, MD, is interim chief of service of ob-gyn at NYU Langone Hospital Brooklyn. She earned her medical degree from SUNY Stony Brook in New York.
Anastasia Matthews, MD, is an ob-gyn at the Ohio State University Wexner Medical Center. She earned her medical degree from Eastern Virginia Medical School in Norfolk, Virginia.
American College of Obstetricians and Gynecologists (ACOG), Ectopic Pregnancy, July 2022
Learn how we ensure the accuracy of our content through our editorial and medical review process.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.