Parents’ Top COVID-19 Questions, Answered
The rapid spread of COVID-19 has parents understandably concerned about their family’s health. And with the situation changing day to day, it’s no wonder we’re bursting with questions. Here, pediatricians tackle the top 12 questions they’ve been getting about the novel coronavirus and how to keep little ones safe.
It’s Said That Kids Aren’t Experiencing Severe Symptoms from COVID-19. What Are Their Symptoms Actually Like?
Symptoms of COVID-19 can often be confused with the flu and include fever, cough, fatigue, achiness, sore throat and diarrhea. If your child is having any signs of trouble breathing (breathing rapidly, short of breath, sucking in the muscles by the ribs/chest), then they should be seen right away by your pediatrician or taken to the ER. But call your doctor’s office first to determine where it’s best for your little one to be looked at.
If your child is a bit congested or has a cough, we recommend just waiting it out. You can try simple at-home remedies, such as having a cool mist humidifier in their room to create moisture, run a steamy shower and sit with your child on the toilet bowl next to the steam to clear their nose, place a few drops of over-the-counter saline drops for kids in each nostril to help relieve congestion, or once in a while use a bulb syringe to remove built-up mucus (we don’t like using suction too much because you can traumatize little noses if your kiddo wiggles away too much).
Try to avoid the doctor’s office during this pandemic as much as possible; instead, talk to your pediatrician over the phone for advice or see if your pediatrician offers telemedicine visits. If, however, you have a young infant, or if your child has a persistent fever more than 72 hours or any other concerning signs such as difficulty breathing, then you should talk to your pediatrician to determine if your child needs a visit.
Many pediatric practices are doing telemedicine and are cutting back right now on seeing well visits that can wait a few weeks. Speak to your pediatrician about what their current office protocol is. For older babies, toddlers and elementary school kids, many pediatricians are okay with delaying vaccines for a few weeks and then catching children up when the pandemic is over. (There are also time ranges in which vaccines can be given and the AAP has guidelines for catching kids up who are delayed).
Many kids are going stir crazy being at home all day, and going outside is an important way to get exercise! Going for walks, hikes, bike rides, scooting or skating in areas that are not crowded or spending time outside in your own backyard are all great activities. If, however, you or your child is sick or has a cough, it’s best to stay inside until they’re all better and fever-free for 72 hours.
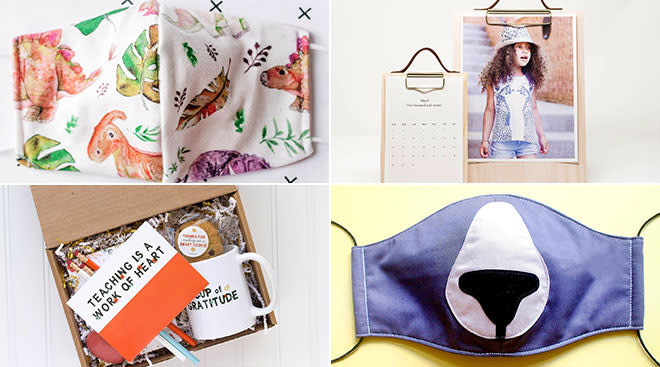
Editor’s note: While the CDC does not recommend that babies and toddlers under 2 wear any face coverings due to the risk of suffocation, they do recommend that kids 2 and older wear a cloth face mask when out in a community setting. That’s because up to 25 percent of people infected with COVID-19 don’t have any symptoms and can unknowingly pass the virus onto others. Don’t have any cloth masks at home? The CDC offers instructions for how to make your own.
We recommend against taking your child to the playground. Many public playgrounds have been closed in the US to help encourage social distancing and prevent the further spread of disease. From what we currently know, the virus can live on surfaces like swings and slides for as long as 48 hours. Try going on family walks or playing with your kids in your own backyard, if you have one.
We understand how important it is for friends and family to meet a new baby. However, given the fact that COVID-19 can be passed even by people who aren’t showing symptoms, we recommend against inviting visitors into your home to prevent you or your little one from getting the disease. This is especially true during the first two months before your child receives vaccines. Any fever has to be taken seriously and requires a trip to the emergency room and additional testing to evaluate the fever.
Although it’s hard, it’s best to practice social distancing right now. Many kids, however, are having fun on “virtual playdates” by FaceTiming with their friends!
There are no remedies that are specific for COVID-19, but it’s good to have on hand some common medicines and supplies if your child becomes sick. Have soap so your kids can wash hands for at least 20 seconds (have your kids sing happy birthday twice), have alcohol-based hand sanitizer with at least 60 percent alcohol, teach your kids not to put their fingers in their mouth or by their face, and to sneeze into a tissue or their elbow. Some studies have demonstrated that using zinc (found in Cold-EEZE and Zicam) could be helpful in decreasing viral symptoms in general and it may also be beneficial with COVID-19 as well. Other common medicines to have on hand are acetaminophen, ibuprofen, Benadryl, OTC hydrocortisone cream, antibiotic ointment, normal saline drops to clear stuffy noses, and an electrolyte solution such as Pedialyte. You should also make sure any medications that your child uses is refilled, such as albuterol for asthma or an EpiPen Jr for anaphylaxis.
We have been asked this question a lot since a recent article raised concerns about the use of ibuprofen (Motrin, Advil) with COVID-19, but the answer is unclear. Based on current information, the World Health Organization doesn’t recommend against using ibuprofen, but they’re consulting with more doctors treating patients with COVID-19 to determine if there are any negative effects. Since we don’t really know the answer, many pediatricians right now advise just using acetaminophen to play it safe (of course, talk to your pediatrician first to get their advice).
Fever is a symptom and tells us something is going on in the body. We often give acetaminophen or ibuprofen (if over 6 months) when a child has a fever to make them more comfortable, but when the medication wears off, the fever may return. There is no height of temperature in children above 8 weeks that requires immediate attention. In babies 0 to 8 weeks old, call your pediatrician immediately if they have a rectal temperature of 100.4 or higher. Most viral fevers last three to five days. But if, along with the fever, your child is having any other serious concerns, like trouble breathing, then your pediatrician should also be alerted right away.
Emergency rooms are very overwhelmed right now, and it’s best not to take your child to one unless completely necessary. Some reasons to go to the ER are if your child is having difficulty breathing (breathing very quickly, audibly wheezing, sucking in the muscles on their chest, grunting or flaring out their nostrils because they’re struggling to breath), a child who is nonresponsive and truly lethargic, a child who has had a bad accident and may have broken bones or a concussion or a child with a new onset seizure. If you’re worried about your child, it’s best to first call your pediatrician, who can advise you over the phone or perhaps refer you for a telemedicine visit rather than going to the ER.
The situation is evolving, and updated recommendations and policies are being implemented on an ongoing basis. For continued up-to-date information, be sure to check the CDC’s guidelines on COVID-19.
About the authors:
Dina DiMaggio, MD, is a pediatrician at Pediatric Associates of NYC and at NYU Langone Medical Center. She has received numerous research awards, along with Patient’s Choice award, compassionate doctor recognition and was featured in the New York Times Magazine as a Super Doctors and New York Rising Star. She and Anthony Porto are coauthors of the book The Pediatrician’s Guide to Feeding Babies and Toddlers.
Anthony Porto, MD, MPH, FAAP, is a pediatrician and pediatric gastroenterologist at Yale New Haven Children’s Hospital and the medical director of the Yale Pediatric Celiac Program. He’s also an associate professor of pediatrics and associate clinical chief of pediatric gastroenterology at Yale School of Medicine. He has won numerous awards including the Norman J. Siegel Award at Yale University for leadership and providing outstanding clinical care as well as Physician of the Year during his time at Morgan Stanley Children’s Hospital. He has been named Castle Connolly Top Doctors since 2012.*
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.