How to Treat a Baby Fever
One unfortunate reality of babyhood is illness, but that doesn’t make dealing with a sick infant any easier. No parent ever wants to see their little one under the weather, so it’s natural for panic to set in the minute baby feels warm to the touch—especially if it’s your little one’s first fever. But the sad fact is that fevers in babies can be common, so they’ll probably have their first high temperature sooner or later. Your best defense is to know what’s considered a fever for a baby and the best course of action to take. Read on for expert advice on how to treat a baby fever, depending on your child’s age and symptoms, as well as when to call the doctor.
You think baby feels warm so you take their temperature—but knowing how to interpret the results is key. So what’s a fever for a baby? A temperature reading of 100.4 degrees Fahrenheit (38 degrees Celsius) or higher is considered a fever in babies. This is not a normal body temperature for babies and therefore constitutes a baby fever, says California-based pediatrician Tanya Altmann, MD. According to the American Academy of Pediatrics (AAP), a normal baby temperature can range from 97 to 100.3 degrees Fahrenheit, depending on how the temperature is taken.
How do you know if it’s a fever or something else that’s bothering baby? One key warning sign of an infant fever is heat. “When baby has a temperature, they feel like a little radiator,” says Rallie McAllister, MD, MPH, a family physician and co-author of The Mommy MD Guide to Your Baby’s First Year. If your child’s forehead feels warm to the touch, use a thermometer to take baby’s temperature (more on that in a bit).
Since your little one can’t tell you when they’re feeling unwell or feverish, it helps to pay attention to their general behavior too. “When baby has a fever, they’ll feed less and either sleep more or sleep less,” Altmann says. “They might be fussier or might not look right at you.” Keep an eye out for the following signs of fever in babies:
- Baby feels warm: “If baby is hotter than usual, that’s a big sign of fever,” McAllister says.
- Changes in behavior: Note how baby is acting. Is something off from their usual temperament? Are they crying a lot or generally being fussy? If so, this could be a sign of baby fever.
- Changes in feeding habits: If baby won’t take a bottle or breast, it could be the reaction to a spike in their temperature.
- Changes in sleeping habits: Again, your little one might be sleeping more—or less—than usual. Both are signs of a potential baby fever.
- Disinterest in playing: If baby doesn’t want to engage or play, it may be a sign that they’re not feeling well.
- Lethargy: If baby is less active than usual, they may be experiencing infant fever.
If your child is 3 months old or younger, take these signs of infant fever very seriously—any sign of increased newborn temperature could indicate a potentially serious illness. Call your pediatrician about a newborn fever ASAP.
Even with all the fancy forehead, ear and under-the-arm thermometers on the market (check out our comprehensive guide), according to the experts, the gold standard for taking baby’s temperature is to use a rectal thermometer. “I usually tell parents there are good forehead thermometers that are perfectly fine for screening a temperature,” Altmann says. “But if that thermometer shows that baby’s temperature is elevated and you call your pediatrician, they’ll still want you to do a rectal reading right away to get a definitive answer.” Look for a digital rectal thermometer with a wide base and a short, flexible tip, which will help keep you from inserting it too far.
Don’t know how to take a baby’s temperature rectally? Place baby on a changing table, add a little dab of petroleum jelly on the end of the thermometer and insert it gently about half an inch into baby’s bottom until it beeps. Then remove it carefully and view the reading.
Forehead temperature (aka temporal artery) offers the second most accurate reading, according to the AAP. Starting when baby is 6 months old, ear temperature (aka tympanic) can also be accurate if taken properly. Armpit temperatures (aka axillary) are the least accurate but can still be used to screen your child; if it comes back with a high temperature, you can turn to the other, more reliable methods to confirm an infant fever. Baby’s temperature shouldn’t be taken orally until they’re 4 years old.
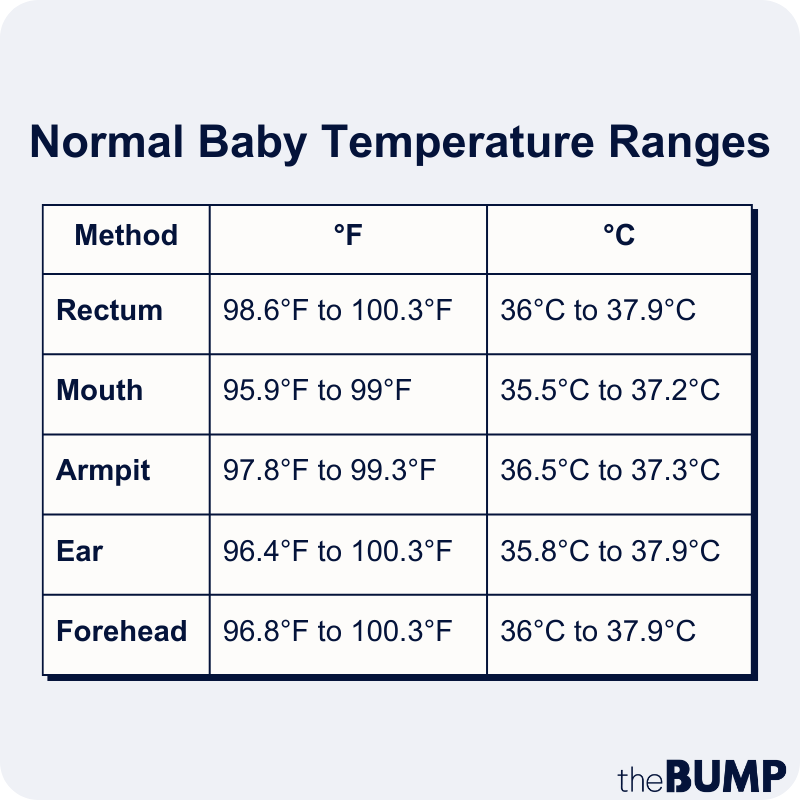
The different methods of taking baby’s temperature not only vary in accuracy, but they also yield different ranges of what’s considered a normal baby temperature. To that end, we’ve included a handy chart to show you normal body temperatures based on whether you’re checking your child’s temperature using the ear, mouth, rectum or armpit. Keep in mind, a normal baby temperature can vary depending on age, activity level and even time of day. According to the AAP, infants often register slightly hotter than older babies, and body temps are generally highest in the late afternoon and early evening and lowest at night and early morning. Below, a handy baby fever chart, from the AAP, Seattle Children’s Hospital and Lauren Crosby, MD, FAAP, a pediatrician based in Beverly Hills, to refer to when taking baby’s temperature:
A high fever in babies can sometimes seem to come out of nowhere, but generally speaking, the causes of a baby fever tend to be very specific. Anything from a virus to an ear infection, urinary tract infection or another more generalized infection could be behind the spike in temperature. “A fever of any origin is a sign you need to take baby to the doctor,” McAllister says. “When they’re 3 months or younger, infant fever is considered a medical emergency.”
Sometimes, though, a high temperature reading is simply caused by overheating. “If baby is over-bundled, that could cause them to feel warm and maybe even exhibit an elevated temperature,” Altmann says. “If a parent calls me and tells me her 2-month-old was swaddled, sleeping, has a temperature of 100.4 degrees but otherwise seems fine, I’ll tell them to unswaddle the baby and retake the temperature in 15 minutes. If it’s truly 100.4 degrees 15 minutes later, then we need to do a work-up. If you unswaddle baby and their temperature is normal and they’re acting fine, I’ll suggest we keep an eye on it, but it’s not as urgent.” In the case of overheating, you can remove excess clothing, move baby to a cooler environment, turn on a fan and even sponge baby down with cool water.
Vaccines can also sometimes cause a low-grade fever in infants. Most of the time your provider will provide you with instructions on how to handle fevers that pop up in the day or two following vaccination. However, if your newborn develops a baby fever after a vaccine and you’re concerned, it’s still a good idea to call your pediatrician. If baby is 4 months or older, a fever of 100.4 to 102 degrees that spikes after a vaccine is nothing to be alarmed about, Altmann says. As long as baby is otherwise acting normal and eating well, you can use a baby fever reducer such as Tylenol (with your pediatrician’s approval) and they’ll likely be back on track pretty quickly. Of course, if baby isn’t acting like themselves, having breathing problems or crying in pain associated with baby fever, call the doctor sooner rather than later.
Can babies get a fever from teething?
Teething may increase baby’s temperature, but only slightly—usually not high enough to be considered a fever. According to Crosby, any fever of 100.4 degrees Fahrenheit or more could be an indication that your child is sick. If baby’s slightly raised temperature appears alongside symptoms such as drooling, swollen gums and the urge to gnaw on things, then teething may be the culprit. Try to make baby comfortable with some tried-and-true remedies, but there’s no reason to panic. However, if baby develops a true fever, teething is likely not the root cause.
Here are some things you can do if you find yourself up in the middle of the night wondering how to bring baby’s fever down. You can certainly discuss using baby fever medicine with your pediatrician, but don’t discount home remedies for baby fever, as they can be effective ways to reduce baby’s temperature. Below, how to reduce a fever in baby naturally:
-
Give an infant fever reducer (if approved by a pediatrician): If baby is under 6 months, call your doctor before giving baby fever medicine, such as Tylenol. Your doctor is likely going to want to examine baby in person to figure out why they’re sick. “For example, if it’s an ear infection, baby will need antibiotics,” McAllister says. Your pediatrician will also want to know exactly how much baby weighs at the time so they can prescribe the correct dosage for a fever reducer.
-
Keep baby hydrated: When your little one has a fever, keeping them hydrated with breast milk or formula is super-important, so you may want to offer extra breast- or bottle-feeding sessions. “Usually babies don’t need other fluids, but speak to your pediatrician to see if baby needs an electrolyte solution,” Altmann says.
-
Consider a sponge bath: This is one of the most effective home remedies for baby fever. Rather than giving baby a full bath where they’re immersed in water, simply give baby a sponge bath to soothe them, dabbing a lukewarm washcloth on their forehead, neck and arms. “Make sure the water is lukewarm, though,” Altmann says. “If the water is too cold it may cause baby to shiver, which could actually elevate the fever.” However, know that you can also give baby a lukewarm bath in a tub to bring their fever down.
-
Dress baby in light layers: Wondering how to dress a baby with fever at night? Opt for lightweight, breathable clothes to help cool them down. Even if your child is experiencing chills, overdressing them may cause baby’s temperature to rise even higher.
-
When in doubt, call your pediatrician: If you’re concerned about baby for any reason, it never hurts to check in with the doctor. If baby is under 3 months, call the doctor no matter what.
The AAP breaks down fever in infants by age and temperature. Follow these expert recommendations on exactly when you should bring a feverish baby to the doctor:
-
Under 3 months: A newborn temperature of 100.4 degrees Fahrenheit or higher must be checked out by a medical professional immediately, since infection can spread more rapidly in a young infant. Call your doctor at the first sign of fever for newborns. “Newborns don’t have the immunity yet that an older baby has so they can get very sick very quickly,” Altmann says.
-
3 to 6 months: When dealing with fever in babies, when to worry at this stage is at 102 degrees or higher. “Babies at this age are better able to deal with a fever,” McAllister says. Still, don’t medicate with Tylenol without your pediatrician’s approval. Instead, call them to discuss fever treatments. Also, if baby’s temperature lasts more than a few days or there are other concerning signs, like baby isn’t drinking fluids, not acting like themselves or is crying or throwing up, seek medical attention immediately.
-
6+ months: If baby has a fever at this age, it’s okay to give Tylenol or Ibuprofen without consulting your doctor—just be sure to follow the instructions and proper dosage. However, if the baby fever continues, or baby pulls at their ears (a possible sign of ear infection), book a pediatrician appointment immediately. “At this age, we’re more concerned about how many days the fever has lasted, the other symptoms the baby has, whether they’re coughing, throwing up, sleeping or drinking fluids,” Altmann says. “If baby is acting fine, we suggest observing the temperature for a few days, but call if the fever lasts longer than three or four days.”
You should also call your pediatrician if baby experiences any of these symptoms along with a fever, regardless of age:
- Vomiting
- Diarrhea
- Seizures (some babies experience seizures triggered by fevers, called febrile seizures)
- Unexplained rash
- Signs of dehydration (i.e. fewer wet diapers, no tears when crying, dry lips or mouth)
- Trouble breathing (breaths that are shallow or slower or faster than normal)
- A change in their skin color
- Extremely lethargic, limp or unable to move
Never hesitate to call the pediatrician if you’re concerned about an increase in baby’s temperature. Whether you’re dealing with an infant fever for the first time or wondering what the cause is of your older baby’s fever, there’s no such thing as being too cautious. The best thing is to be informed, so you can confidently care for your little one and get them back to their happy, healthy self.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Tanya Altmann, MD, FAAP, is a Los Angeles–based pediatrician and a spokesperson for the American Academy of Pediatrics. In addition to founding Calabasas Pediatrics, she's also an assistant clinical professor at Mattel Children’s Hospital at UCLA. Altmann has authored several books, including Baby and Toddler Basics: Expert Answers to Parents’ Top 150 Questions(https://www.amazon.com/Baby-Toddler-Basics-Answers-Questions/dp/1610021266?&linkCode=ll1&tag=tb-baby-fever-20&linkId=5f4385fd8a5bcbc4648668c589ad1d5f&language=en_US&ref=asli_ss_tl) and What to Feed Your Baby: A Pediatrician’s Guide to the 11 Essential Foods to Guarantee Veggie-Loving, No-Fuss, Healthy-Eating Kids(https://www.amazon.com/What-Feed-Your-Baby-Healthy-Eating/dp/0062404946?&linkCode=ll1&tag=tb-baby-fever-20&linkId=0244172d78aeb9c339184c208f6a1445&language=en_US&ref=asli_ss_tl). She earned her medical degree from Sackler School of Medicine in New York City.
Lauren Crosby, MD, FAAP, is a pediatrician with La Peer Pediatrics in Beverly Hills, California, as well as a mom of two. She earned her medical degree from UCLA School of Medicine and completed her residency at Cedars-Sinai Medical Center. She currently serves as an official spokesperson for the American Academy of Pediatrics.
Rallie McAllister, MD, MPH, is a family physician with over two decades of experience, as well as a nationally recognized health expert. She is also the cofounder of The Mommy MD Guides and coauthor of The Mommy MD Guide to Your Baby’s First Year(https://www.amazon.com/Mommy-Guide-Your-Babys-First/dp/B01D3Q6AKQ?&linkCode=ll1&tag=tb-baby-fever-20&linkId=2586ca2b50c6553b3f64b1862ba9cfaf&language=en_US&ref=asli_ss_tl).
American Academy of Pediatrics, Fever and Your Baby, July 2021
Seattle Children’s Hospital, Fever (0-12 Months), October 2023
American Academy of Pediatrics, How to Take Your Child’s Temperature, October 2020
Learn how we ensure the accuracy of our content through our editorial and medical review process.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.