Signs of Miscarriage: Everything You Need to Know
Miscarriage is more common than you might think. According to experts, about 10 to 25 percent of pregnancies will result in a miscarriage. Still, many couples find it difficult to talk about pregnancy loss, and instead face their grief and frustration alone. Ultimately, this means less awareness around the topic, which can make it even more scary and confusing for those going through the experience.
It’s not particularly light or uplifting, but some basic education around the often taboo topic of miscarriage can help you navigate this tricky terrain. What’s more, it can serve as a reminder that you’re not alone. In our guide, we’re sharing everything you need to know about miscarriage. We’ll help you understand what a miscarriage is and why it happens, learn to recognize symptoms and signs of miscarriage and find out how to cope with all the emotions that accompany the loss of a pregnancy.
Miscarriage is the medical term used when a pregnancy spontaneously ends before the 20th week. Still, there are many different types of miscarriage, depending on when and how it happens. To help with the confusion, here’s a look at the specific meanings behind some different types of miscarriage.
Chemical pregnancy
A chemical pregnancy is a very early miscarriage that happens before 5 weeks gestation. It occurs when the embryo hasn’t properly attached to the uterine wall. It’s possible you may think you’re pregnant based on symptoms like a missed period (or a positive pregnancy test), but these chemical pregnancies, which account for up to 75 percent of all miscarriages, are lost so early after implantation (usually just two weeks after) that the bleeding can be mistaken for your period. Many women don’t even realize they were ever pregnant.
Missed miscarriage
A missed miscarriage, also sometimes known as a silent miscarriage or missed abortion, can happen anytime prior to week 20 when an embryo or fetus dies but the body hasn’t recognized the loss or gotten rid of the pregnancy tissue. Since the placenta may still continue to release hormones, some women keep having pregnancy symptoms, but others may sense those symptoms fade and experience a brownish discharge. A missed miscarriage is often diagnosed during a checkup, when a doctor no longer finds a heartbeat.
Threatened miscarriage
A threatened miscarriage is your body’s way of giving you a warning sign that miscarriage is a possibility during the first three months. You may experience symptoms of vaginal bleeding and abdominal pain, but the cervix stays closed and a heartbeat remains. Your doctor will likely recommend pelvic rest and that you avoid or restrict certain activities until you’re in the clear. The majority of women who have a threatened miscarriage will go on to have a healthy pregnancy.
Incomplete miscarriage
An incomplete miscarriage happens when your body only pushes out some of the pregnancy tissue. Symptoms include bleeding, cramping and a dilated cervix. A pregnancy test might still be positive but the fetus is no longer viable. Most of the time an incomplete miscarriage will become complete on its own, but you may need medical intervention to help remove the remaining tissue.
Blighted ovum
Your doctor may call this an “anembryonic pregnancy,” and it almost always happens in the first trimester. It means that the fertilized egg attached to the wall of your uterus, but while it may have begun to form a placenta, it never developed into an embryo.
For healthy women in the US, the miscarriage risk is anywhere from 10 to 25 percent, according to the American Pregnancy Association. As you get older, your miscarriage risk, not surprisingly, goes up. Once you hit 35, the odds increase to 20 to 35 percent, and up to 50 percent at age 45. Keep in mind that most miscarriages happen in the first trimester (before 13 weeks of pregnancy), with only about 1 to 5 percent occuring during the second trimester (between weeks 14 and 20).
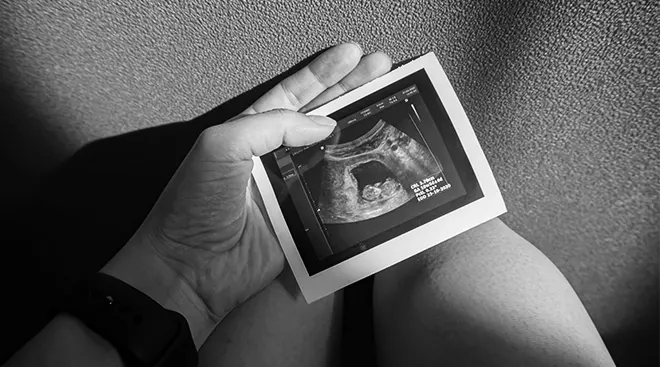
Here’s the good news: According to a study, after an ultrasound confirms baby’s heartbeat at eight weeks, the risk of miscarriage is about 3 percent. Better yet, research published in Obstetrics & Gynecology indicates that the rate is closer to 1.6 percent for women experiencing no symptoms. What’s more, the risk of miscarriage continues to fall even lower as the weeks progress—so try not to stress.
It can be scary if you start experiencing miscarriage symptoms. So how do you know if you’re actually having a miscarriage? You may be surprised to hear that a miscarriage can unfold over several hours, days or sometimes even weeks. It typically starts with common miscarriage symptoms like cramping in your pelvis or lower back and possibly vaginal bleeding.
If you’re bleeding in the first trimester of pregnancy, though, don’t panic; according to the American Pregnancy Association, about half the time, this miscarriage symptom actually stops, and the pregnancy continues to term. In some cases, there aren’t any warning signs of miscarriage until an ultrasound shows no heartbeat. That said, the following can be common miscarriage symptoms:
Heavy bleeding
Bleeding or spotting is the most common sign of an early miscarriage. Remember, many women experience spotting—light bleeding, typically pink or brown discharge—up until the 14th week of pregnancy, so don’t jump to conclusions. “A little bleeding doesn’t necessarily mean you’re going to have a miscarriage,” says Caroline Conner, MD, an ob-gyn at Orange Coast OBGYN in Fountain Valley, California. Call your doctor if the bleeding is bright red, similar to a light period. If you’re experiencing symptoms of heavy bleeding, passing clots or tissue and/or if you feel dizzy or faint during pregnancy, head to the nearest emergency room.
Loss of pregnancy symptoms
Sometimes, the only sign of miscarriage is the sudden disappearance of pregnancy symptoms, such as morning sickness and breast soreness. If you suddenly notice that your pregnancy symptoms have gone away, see your doctor for an ultrasound.
Pain or cramping in the center of the lower abdomen or back
Occasional back discomfort is normal during pregnancy, but if the pain persists, don’t ignore it—especially if it’s stronger than normal period cramps. Cramping, along with spotting, is among the more common signs of early miscarriage.
White-pink discharge
A light pink, mucus-like vaginal discharge may be a miscarriage symptom. This can be misleading, though, since many women experience discharge during a normal, healthy pregnancy.
Weight loss
Weight loss in pregnancy after steady weight gain is a possible but atypical sign of miscarriage. Of course, it’s much more likely that morning sickness would be what triggers mild weight loss, says Heather Bartos, MD, an ob-gyn and the medical director of Be. Women’s Health and Wellness in Frisco, Texas.
Painful contractions
Some women experience more than just cramping. If you’re having painful contractions 5 to 20 minutes apart, this could be a sign of premature labor.
Decreased fetal movement
If you’re later in your pregnancy and notice a sudden or significant decrease in baby’s activity, you may be experiencing a late miscarriage. If you notice this miscarriage symptom, contact your doctor right away.
In addition to these physical symptoms, some women intuitively know that something is wrong. They’re able to sense that they’re no longer pregnant. Of course, this may be explained by a sudden stop to certain symptoms, but there could be more to it. “I have many women who are not bleeding say, ‘I just don’t feel pregnant anymore,’” says Stephanie McClellan, MD, an ob-gyn at Hoag Hospital in Newport Beach, California. “There is communication between the mother and developing fetus—we don’t understand it completely, but these women are almost always right.” Trust your instinct, and don’t shrug off this potential sign of a miscarriage.
That said, it’s also possible to experience a miscarriage without realizing it. “Sometimes the most common symptom is no symptoms; a miscarriage is just found in the doctor’s office when a routine sono is done. This is called a ‘missed miscarriage.’” says Bartos.
What to do if you’re experiencing miscarriage symptoms
If you’re experiencing any of the above potential miscarriage symptoms—or any abnormal pregnancy symptoms, for that matter—call your doctor. “We have a motto in our practice,” McClellan says. “We tell our patients: We’d rather hear from you 100 times too many than one time too little.” Remember, there may be other explanations for physical symptoms; your body is going through a lot of change right now. So keep calm, and check in with your ob-gyn.
Unfortunately, if you’re experiencing a miscarriage, there’s nothing you can do to stop or prevent it. Because a miscarriage can cause an infection or hemorrhaging, your doctor will want to assess you and provide next steps.
Now that you know the possible signs of miscarriage, you’re probably wondering how it feels. The amount of pain associated with miscarriage can vary from woman to woman. Many feel nothing and don’t even realize it’s happening; others experience a range of aches and cramps, from mild to strong, like a really bad period. Some women even report experiencing full-on, painful labor contractions that last for hours or even days. If the pain is intense, the bleeding is heavy (you’re soaking a pad every hour) or the remains of the pregnancy don’t pass completely (an ultrasound will confirm this), your doctor may perform a D&C (dilation and curettage) or, if you’re beyond the 14-week mark, a D&E (dilation and evacuation).
As Tannaz Ebrahaimi Adib, MD, an ob-gyn at Tri-City Medical Center in Oceanside, California, explains, these brief surgical procedures will put an end to cramps and bleeding and help prevent an infection, which may happen if any of that tissue remains behind in the uterus. Both procedures are typically done in a hospital or surgical center, and you’ll either get local or general anesthesia, so you shouldn’t feel anything. Unless there are complications (which are rare), you can usually go home the same day. Expect some strong cramping the first 24 hours after the procedure—that’s totally normal—and then mild cramping and light spotting for a few days up to two weeks. Taking Tylenol or Advil can help alleviate any post-procedure pain.
Experiencing the loss of a pregnancy can be devastating, and you’ll probably have a lot of questions, including “why did this happen?” It’s not uncommon to start blaming yourself, but most miscarriages happen in the first trimester of pregnancy for reasons that are beyond your control. In the majority of cases, there’s no way to prevent a miscarriage and nothing you could or should have done differently.
Below are three of the most common miscarriage causes.
Chromosomal abnormalities
More than half of early miscarriages are the result of a chromosomal abnormality, when the sperm and egg come together but one of them has too many or too few chromosomes, those tiny structures in each cell that carry our genes. In other instances, the 23 pairs of chromosomes from each parent fail to line up properly. Either way, the embryo isn’t genetically strong enough to sustain a viable pregnancy.
Medical disorders
Chronic medical conditions such as blood clotting disorders, thyroid disease and diabetes can increase your risk of miscarriage. Certain autoimmune diseases, such as lupus, can also directly affect pregnancy. That doesn’t mean that if you have an autoimmune problem, you can’t deliver a healthy baby. Talk to your doctor about the risks of miscarriage and complications, and the best ways to plan for pregnancy.
Uterine abnormalities
Things like a uterine septum (a dividing wall in the uterus) or any anatomic abnormalities such as a small or misshapen cavity, endometrial polyps or fibroids account for about 10 percent of recurrent miscarriages, particularly after the first trimester of pregnancy. An ob-gyn should be able to identify these issues and determine whether there are ways to help you achieve a healthy pregnancy. Another possible cause of miscarriage in the second trimester of pregnancy is a weakened cervix. Normally during pregnancy, the cervix (the lower part of the uterus that connects to the vagina) is closed and rigid. But sometimes it can begin to open too early. If your cervix starts opening prematurely, or if you know you’re at risk for weakened cervix, your ob-gyn may recommend certain medications, frequent ultrasounds and a procedure called cerclage, which closes up the cervix with strong sutures.
There are a few other factors that could potentially increase your risk of miscarriage. As previously noted, as a woman gets older, her chance of miscarriage goes up. Those who are significantly overweight or underweight may also be at greater risk. Finally, doctors warn that certain unhealthy lifestyle habits, such as smoking cigarettes, using illicit drugs and drinking heavily in pregnancy can increase the chances of miscarriage as well.
Can stress cause miscarriage?
There’s no evidence that stress directly affects your risk of miscarriage, but it may play a role. Research shows that a mother’s physical and emotional state—including her fitness level and quality of nutrition—can raise or lower her level of stress sensitivity, potentially influencing everything from fertility and conception to the quality of the placenta and the risk for premature labor. McClellan recommends focusing on nutrition, exercise (approved by your doctor) and mind-body relaxation, especially in the first and second trimesters of pregnancy. But there’s no need to check yourself into a month-long spa retreat (well, unless you want to!). It could be as simple as taking an extra 15 minutes after lunch to listen to some relaxing music, decompress and let your body absorb the nutrients you’ve just eaten.
Risk of miscarriage for twin pregnancies
While multiple gestations can carry greater risk of complications, the rate of miscarriage is about the same in twin pregnancies as it is in singleton pregnancies. “Miscarriage risk can be anywhere from 15 to 25 percent, depending on a woman’s age and medical history. Having another baby in the uterus is independent in that number (meaning that each baby has a chance of miscarriage). In some cases, one twin can miscarry or simply ‘vanish,’ leaving a surviving twin. This is also known as vanishing twin syndrome,” explains Bartos.
A study found that the overall occurrence of miscarriage in twins pregnancies may hover around 17 percent (12 percent vanishing twins and 5 percent total miscarriages). That makes the risk per gestational sac about 11 percent. Again, this incidence rate drops once fetal heartbeats are detected.
Experiencing multiple miscarriages
In most cases, having one miscarriage doesn’t mean you’re at risk for another. “Just because you had one miscarriage might not mean you can’t have healthy baby,” Conner says. Doctors are more concerned if they see a pattern of two or more consecutive miscarriages in the first trimester of pregnancy or one second trimester miscarriage. That’s when you may be considered at a higher risk for miscarriage in additional pregnancies. If you’ve had two or more miscarriages, see your doctor to check for an underlying cause of miscarriage, such as fibroids, polyps, endometriosis or uterine abnormalities.
Different people handle miscarriage in different ways, but it’s not uncommon to feel devastated as you would after any other loss in your life. If you’re having trouble coping with a miscarriage or it’s causing a rift in your relationship with your partner, ask your doctor for a referral to a therapist for counseling services. Then read about some ways to honor your loss and slowly begin to move on when you’re ready.
How quickly you can try to get pregnant again after a miscarriage depends on a few physical and emotional factors. Every case is different, and you should only start trying to conceive once your doctor has given you the green light. “I usually tell patients to wait until their next normal cycle, anywhere from four to six weeks after miscarriage,” Conner says. If you want to wait longer, that’s totally normal too—in fact, some providers may recommend waiting up to three months to allow for recovery. What’s most important is you give your mind and body the time they need to heal, and you’ll know when you’re ready to try again.
Miscarriages happen. It doesn’t mean you did anything wrong, and it certainly doesn’t make you a failure. Understanding what it entails, why it occurs and how you can move forward after miscarriage will hopefully help you feel supported. There’s no shame or stigma, so reach out for help if you need it.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
Tannaz Ebrahaimi Adib, MD, os an ob-gyn at Tri-City Medical Center in Oceanside, California. She received her medical degree at Shahid Beheshti University of Medical Sciences in Iran.
Heather Bartos, MD, is an ob-gyn and the medical director of Be. Women’s Health and Wellness in Frisco, Texas. A navy veteran, she spent 12 years serving the women and spouses of the armed forces, and was an associate professor at the Uniformed Services University of Health Sciences in Bethesda, Maryland. She completed her residency at Baylor College of Medicine, and earned her medical degree at The University of Texas.
Caroline Conner, MD, is an ob-gyn at Orange Coast OBGYN in Fountain Valley, California. She received her medical degree at the University of Texas in Houston, Texas.
Stephanie McClellan, MD, is an ob-gyn at Hoag Hospital in Newport Beach, California. She earned her medical degree at the University of Southern California, Kerk School of Medicine in Los Angeles, California.
American Pregnancy Association, Symptoms & Signs of Miscarriage
JAMA, Low fetal loss rates after ultrasound-proved viability in early pregnancy, November 1987
Obstetrics & Gynecology, Miscarriage Risk for Asymptomatic Women After a Normal First-Trimester Prenatal Visit, March 2008
American Pregnancy Association, Bleeding During Pregnancy
Human Reproduction, Risk of spontaneous abortion in singleton and twin pregnancies after IVF/ICSI, August 2003
Learn how we ensure the accuracy of our content through our editorial and medical review process.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.